What Is Palliative Care At Home: What To Expect?
In this article, we will explore what to expect when receiving palliative care at home.

Palliative Care at Home: Providing Serenity
When faced with a serious illness or end-of-life care, palliative care at home can provide a comforting and supportive environment for both patients and their families. This specialized form of care focuses on improving the quality of life and managing symptoms, ensuring that individuals receive the physical, emotional, and psychological support they need.

Understanding Palliative Care at Home
Palliative care at home is a holistic approach to caring for individuals with serious illnesses. It aims to alleviate pain, manage symptoms, and provide emotional support, all within the comfort of one's own home. This form of care is not limited to a specific disease or condition and can be provided at any stage of a serious illness.
The goal of palliative care at home is to enhance the overall well-being of the patient and promote their comfort and dignity. It involves a multidisciplinary team of healthcare professionals, including doctors, nurses, caregivers, and supportive services. This team works collaboratively to develop personalized care plans tailored to the unique needs and goals of each individual.
What to Expect from Palliative Care at Home
Palliative care at home offers a range of services to meet the physical, emotional, and social needs of patients and their families. Here are some key aspects you can expect from palliative care at home:
Physical Comfort and Symptom Management
Palliative care at home focuses on comprehensive pain and symptom management, ensuring that individuals are as comfortable as possible. This may involve the use of medications, therapies, and other interventions to alleviate pain, manage symptoms, and improve overall physical well-being. Pain management strategies may include the use of analgesics, physical therapy, or other techniques tailored to the patient's needs.
To address physical symptoms, the palliative care team may provide assistance with activities of daily living (ADLs), such as bathing, dressing, and feeding. They may also coordinate the delivery of medical equipment or supplies, such as mobility aids or specialized mattresses, to ensure the patient's safety and comfort.
Emotional and Psychological Support
Palliative care at home recognizes the importance of emotional and psychological well-being for patients and their families. Counseling and therapy services may be offered to help individuals cope with the emotional challenges that arise during the course of serious illness. Grief and bereavement support may also be provided to both patients and their loved ones, ensuring that they have the necessary support during difficult times.
Personalized Care Plans
Each patient's journey is unique, and palliative care at home acknowledges this by creating personalized care plans. These plans take into account the individual's physical condition, personal preferences, and goals of care. The interdisciplinary team collaborates to develop a tailored approach that aligns with the patient's wishes and respects their values and beliefs.
By providing palliative care at home, patients have the opportunity to receive specialized care in a familiar and comfortable environment, surrounded by loved ones. This form of care allows individuals to maintain their sense of autonomy and independence while receiving the necessary support to enhance their quality of life.
Palliative care at home offers a compassionate and holistic approach to care, focusing on physical comfort, emotional well-being, and personalized support.
The Role of the Palliative Care Team
When it comes to palliative care at home, a dedicated team of healthcare professionals plays a crucial role in providing compassionate and comprehensive care. This team consists of caregivers, nurses, and supportive services, all working together to ensure the best possible quality of life for patients and their families.
Caregivers and Nurses
Caregivers and nurses form the backbone of the palliative care team, providing hands-on care and support to patients at home. These skilled professionals are trained in delivering personalized care and addressing the specific needs of each individual.
Caregivers play an essential role in assisting with activities of daily living (ADLs), such as bathing, dressing, and meal preparation. They provide emotional support, companionship, and help create a comfortable and nurturing environment for patients. Additionally, caregivers offer respite care to relieve family members or primary caregivers who may need a break. Their presence ensures that patients receive the attention and care they need around the clock.
Nurses, on the other hand, bring specialized medical knowledge and expertise to the palliative care team. They assess the patient's condition, manage medications, and monitor symptoms. Nurses also collaborate with other healthcare professionals to develop and implement personalized care plans. Their role extends beyond physical care, as they provide emotional support, education, and guidance to patients and their families.
Supportive Services
Supportive services are an integral part of palliative care at home, offering additional assistance and resources to patients and their families. These services are designed to address the various needs and challenges that arise during the palliative care journey.
Supportive services may include:
- Social workers: These professionals provide emotional support, counseling, and help navigate the complex healthcare system. They assist patients and families in accessing community resources, financial assistance, and other support programs.
- Chaplaincy services: Palliative care often recognizes the importance of spirituality and religion in the lives of patients. Chaplains provide spiritual and existential support, helping patients find comfort and meaning during difficult times.
- Volunteers: Trained volunteers offer companionship, respite care, and practical assistance. They provide a comforting presence, engage in conversation, and offer a helping hand to patients and families.
- Therapists: Occupational therapists and physical therapists may be part of the supportive services team, helping patients maintain their independence and functionality. They provide guidance on exercises, mobility aids, and home modifications to ensure a safe and comfortable living environment.
By working collaboratively, the palliative care team ensures that patients receive holistic and compassionate care tailored to their needs. This multidisciplinary approach provides a comprehensive support system that addresses not only the physical aspects of care but also the emotional, social, and spiritual well-being of patients and their families.
Note: The specific composition of the palliative care team may vary based on the healthcare provider and the unique needs of the patient.
Comprehensive Pain and Symptom Management
One of the primary goals of palliative care at home is to provide comprehensive pain and symptom management for individuals with serious illnesses. This specialized form of care focuses on improving the quality of life for patients by addressing their physical and emotional needs. Let's take a closer look at the pain management strategies and ways to address physical symptoms in palliative care at home.
Pain Management Strategies
Pain management is a cornerstone of palliative care. The palliative care team, which may include doctors and nurses, works closely with patients and their families to develop personalized pain management plans. The primary objective is to alleviate pain and provide comfort to patients who are experiencing physical discomfort.
Pain management strategies in palliative care at home may include:
- Medications: The use of analgesics, such as opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), and adjuvant medications, to manage pain.
- Dosage adjustments: The palliative care team regularly assesses and adjusts medication dosages to ensure optimal pain control while minimizing side effects.
- Non-pharmacological interventions: Techniques such as relaxation exercises, massage therapy, and heat or cold therapy may be employed to complement medication-based pain management.
Addressing Physical Symptoms
In addition to pain management, palliative care at home also focuses on addressing a range of physical symptoms that can arise from a serious illness. The palliative care team collaborates with patients and their families to identify and manage these symptoms, aiming to improve the patient's overall comfort and well-being.
Physical symptoms that may be addressed in palliative care at home include:
- Nausea and vomiting: Medications and antiemetics can help manage these symptoms and improve the patient's appetite and quality of life.
- Shortness of breath: Palliative care professionals may use medications and breathing techniques to alleviate respiratory distress and enhance comfort.
- Fatigue: Strategies such as energy conservation techniques, activity pacing, and managing sleep disturbances can help reduce fatigue and improve daily functioning.
- Constipation: The palliative care team may recommend dietary modifications, hydration, and laxatives to relieve constipation and promote regular bowel movements.
By implementing comprehensive pain and symptom management strategies, palliative care at home aims to enhance the well-being of patients with serious illnesses. The care team works closely with patients and their families to ensure that any physical discomfort is effectively managed, allowing patients to experience maximum comfort and maintain the highest possible quality of life.
Note: The specific pain management strategies and approaches for addressing physical symptoms may vary depending on the individual needs and condition of the patient. The palliative care team tailors the treatment plan to provide personalized care that meets the unique requirements of each patient.
Emotional and Psychological Support
When receiving palliative care at home, emotional and psychological support play an integral role in ensuring the overall well-being of the patient and their family. The emotional and psychological aspects of care are just as important as the physical aspects, as they address the unique challenges and emotions that arise during this time. Palliative care at home provides various services to help individuals and their families navigate these complex emotions.
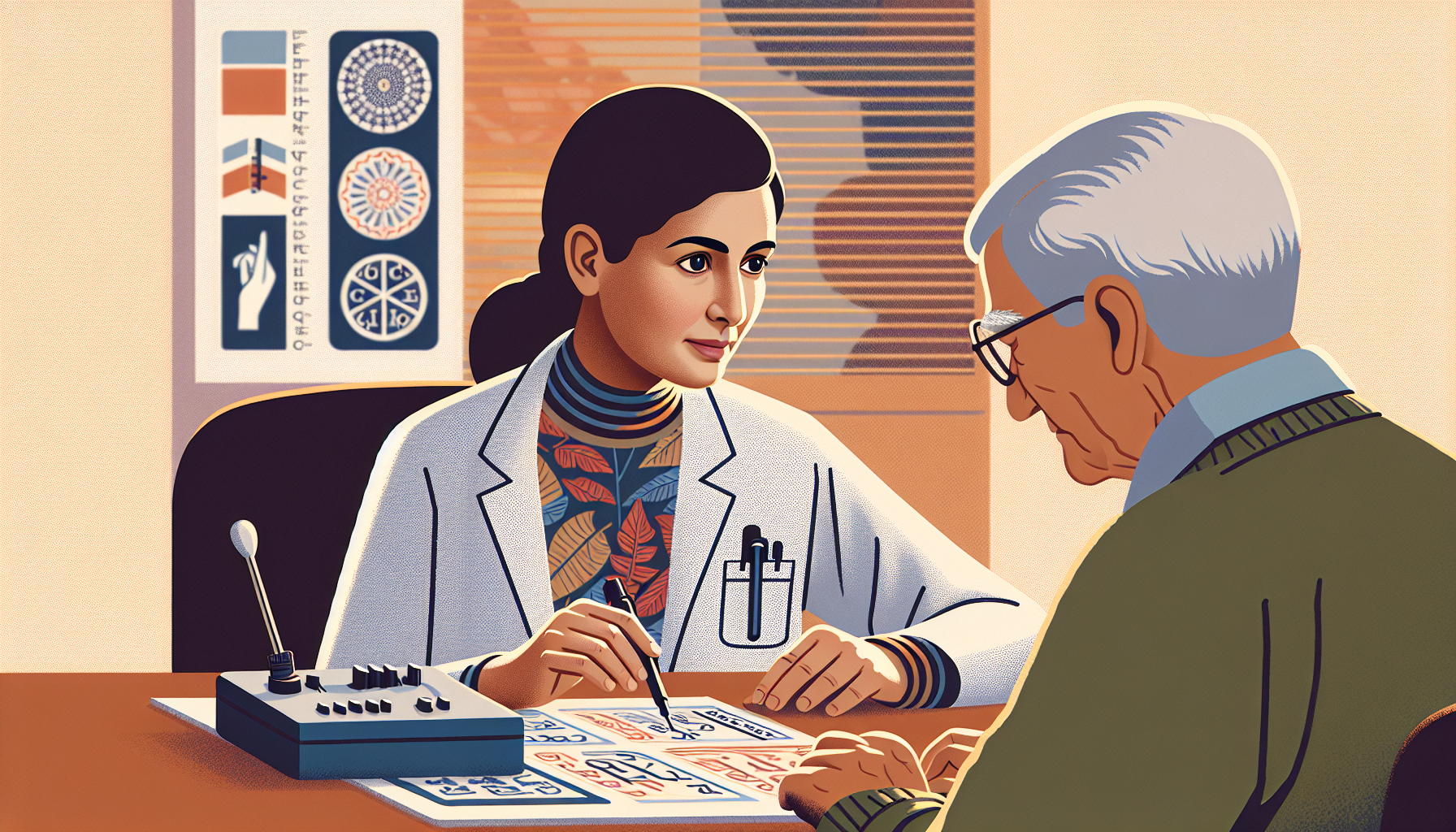
Counseling and Therapy
Counseling and therapy are important components of emotional and psychological support in palliative care at home. Trained professionals, such as psychologists or counselors, work closely with patients and their families to provide a safe and supportive environment for expressing their feelings, fears, and concerns. These professionals can help individuals cope with the emotional challenges that come with a serious illness or end-of-life care.
Through counseling and therapy, patients and their families can gain valuable support, learn effective coping strategies, and develop resilience during this difficult time. It provides an opportunity to address the emotional impact of the illness, discuss fears and anxieties, and explore ways to improve overall well-being. Palliative care providers may offer access to counseling and therapy services or refer individuals to appropriate mental health professionals in the community.
Grief and Bereavement Support
Grief and bereavement support are essential components of palliative care at home, both during the patient's life and after their passing. Palliative care teams understand that the grieving process extends beyond the loss itself, and they provide ongoing support to families during this challenging time.
Grief support may involve individual counseling, support groups, or other resources to help individuals navigate their emotions and adjust to life after the loss of a loved one. These services provide a space for individuals to express their grief, share experiences with others who have gone through similar situations, and access professional guidance as needed.
By addressing the emotional and psychological needs of patients and their families, palliative care at home aims to provide comprehensive support throughout the entire care journey. Counseling, therapy, and grief and bereavement support services contribute to the overall well-being and quality of life for those receiving palliative care at home.
Enhancing Quality of Life
When receiving palliative care at home, the focus is on enhancing the quality of life for individuals with serious illnesses. This involves personalized care plans and assistance with activities of daily living to ensure comfort and support.
Personalized Care Plans
A key aspect of palliative care at home is the development of personalized care plans. These plans are tailored to meet the unique needs and preferences of the individual receiving care. The care team, which may include caregivers, nurses, and other healthcare professionals, works closely with the patient and their family to create a comprehensive plan that addresses physical, emotional, and spiritual aspects of care.
Personalized care plans take into consideration the individual's medical condition, symptoms, and goals of care. They outline the specific interventions, treatments, and therapies that will be provided to manage symptoms, alleviate pain, and improve overall well-being. These plans are regularly reviewed and adjusted as needed to ensure they remain aligned with the individual's changing needs.
Assistance with Activities of Daily Living
In addition to personalized care plans, palliative care at home also offers assistance with activities of daily living (ADLs). ADLs refer to the routine activities that individuals need assistance with due to their illness or physical limitations. Examples of ADLs include bathing, dressing, grooming, mobility assistance, and meal preparation.
Caregivers and healthcare professionals trained in palliative care provide compassionate support and assistance with these activities. They work closely with the individual and their family to ensure a safe and comfortable environment that promotes independence and dignity. This assistance not only helps individuals with their physical needs but also provides emotional support and companionship.
By offering personalized care plans and assistance with activities of daily living, palliative care at home aims to improve the quality of life for individuals and their families. This comprehensive approach to care recognizes the unique needs of each person and strives to provide comfort, support, and serenity during a challenging time.
Holistic Approach to Care
When it comes to providing palliative care at home, a holistic approach is essential to address the physical, emotional, and spiritual needs of the individual. By incorporating complementary therapies and offering support for spiritual and existential needs, palliative care teams strive to enhance the overall well-being and quality of life for patients and their families.
Complementary Therapies
Complementary therapies play a vital role in palliative care at home by providing additional support to manage symptoms, reduce stress, and improve overall comfort. These therapies are used alongside traditional medical treatments and can vary based on individual preferences and needs. Some commonly employed complementary therapies include:
- Massage Therapy: Gentle massage techniques can help alleviate muscle tension, promote relaxation, and provide a sense of comfort.
- Aromatherapy: The use of essential oils, such as lavender or chamomile, can help relieve anxiety, improve sleep, and enhance emotional well-being.
- Music Therapy: Listening to soothing music or engaging in musical activities can bring a sense of peace, reduce pain perception, and encourage emotional expression.
- Art Therapy: Engaging in creative activities, such as painting or drawing, can serve as a form of self-expression, stress relief, and emotional exploration.
- Pet Therapy: Interacting with trained therapy animals can offer companionship, emotional support, and a source of joy and comfort.
These complementary therapies are tailored to meet the unique needs of each individual and are provided in collaboration with the palliative care team. They can contribute to a more holistic and comprehensive approach to care.
Support for Spiritual and Existential Needs
Recognizing and addressing the spiritual and existential needs of individuals receiving palliative care at home is an integral part of the holistic approach. Palliative care teams understand that spirituality and meaning-making play significant roles in the lives of patients and their families, particularly during this time.
Support for spiritual and existential needs may include:
- Pastoral Care: Access to spiritual leaders, chaplains, or clergy who can provide guidance, support, and religious or spiritual rituals based on individual beliefs.
- Counseling and Emotional Support: Engaging in discussions about life, meaning, and purpose, allowing individuals to explore their emotions and find support during challenging times.
- Assistance with Advance Care Planning: Helping patients and their families navigate decisions related to end-of-life care, including clarifying values, discussing preferences, and completing advance directives.
By addressing the spiritual and existential dimensions of care, palliative care teams ensure that patients and their families receive support and guidance throughout their journey.
Through the incorporation of complementary therapies and support for spiritual and existential needs, palliative care at home aims to provide a comprehensive and holistic approach to care. By addressing the physical, emotional, and spiritual aspects of individuals and their families, palliative care teams strive to create an environment of comfort, serenity, and support during challenging times.
FAQs
How is palliative care at home different from hospice care?
Palliative care can be provided at any time during a serious illness, while hospice care is typically reserved for those who are nearing the end of their lives. Additionally, hospice care is usually only provided in the patient's home or in a specialized facility, while palliative care can be provided in a variety of settings.
Will my insurance cover palliative care at home?
Most insurance plans, including Medicare and Medicaid, cover some or all of the costs associated with palliative care. Your healthcare provider can help you understand what your insurance will cover.
Do I need to have a serious illness to receive palliative care?
Yes, palliative care is intended for patients with serious illnesses. However, it can be provided at any stage of the illness and alongside curative treatments.
Can I still see my regular doctor if I receive palliative care at home?
Yes, you can continue to see your regular doctor while receiving palliative care. In fact, your regular doctor may work closely with your palliative care team to ensure that you receive comprehensive and coordinated medical treatment.
How long can I receive palliative care at home?
The length of time that you receive palliative care depends on your individual needs and preferences. Some patients receive palliative care for several weeks or months, while others may receive it for several years. Your healthcare provider will work with you to determine what is best for you and your family.
Summary
Palliative care can be a valuable resource for patients and families facing serious illnesses. When receiving palliative care at home, you can expect a care plan tailored to your needs, a team of care providers, symptom management, emotional support, and 24/7 availability. By understanding what to expect from palliative care at home, you can make an informed decision about the best care options for your loved one.