How Eyes Can Reveal Early Signs Of Alzheimer's?
Let's learn more about the early signs of Alzheimer's revealed through ocular biomarkers.

Recognizing Alzheimer's Early Signs
Early detection of Alzheimer's disease is crucial for providing timely care and support to individuals affected by this progressive neurological condition. By being aware of the early signs, caregivers can take necessary steps to ensure their loved ones receive the appropriate care. Two common early signs of Alzheimer's disease are memory and cognitive decline, as well as challenges with daily tasks.
Memory and Cognitive Decline
One of the most common signs of Alzheimer's disease is the decline in memory and cognitive function. Individuals may begin to forget recently learned information, important dates or events, and may ask the same questions repeatedly. They may also increasingly rely on memory aids or family members for tasks they used to handle independently. These memory lapses and difficulties in retaining new information can be early indicators of Alzheimer's disease.
Challenges with Daily Tasks
In addition to memory and cognitive decline, individuals with Alzheimer's disease may face challenges when performing daily tasks. Simple activities that were once routine may become increasingly difficult. For example, they may have trouble driving to a familiar location, organizing a grocery list, or remembering the rules of a favorite game. These difficulties can impact their independence and quality of life.
It's important for caregivers to be observant and proactive in recognizing these early signs. If you notice these changes in your loved one, it may be beneficial to consult a healthcare professional for a comprehensive evaluation. Early diagnosis can help in developing appropriate care plans and accessing support services to manage the progression of the disease.
Vision Changes in Alzheimer's
Alzheimer's disease is a neurodegenerative condition that affects not only memory and cognition but also various aspects of vision. Understanding the vision changes associated with Alzheimer's can be essential for caregivers in providing appropriate support. In this section, we will explore two common vision changes in individuals with Alzheimer's: the impact on driving abilities and difficulty with visual perception.
Impact on Driving Abilities
One of the early signs of Alzheimer's disease can be a decline in driving abilities. As the disease progresses, individuals may experience difficulties with various aspects of driving, including judging distances, maintaining focus, and responding to traffic signs or signals. These vision-related challenges can compromise their safety and the safety of others on the road.
It is crucial for caregivers to monitor and assess the driving abilities of individuals with Alzheimer's regularly. If there are concerns about their safety, it may be necessary to limit or discontinue their driving privileges. Encouraging alternative transportation options, such as carpooling, using public transportation, or relying on designated drivers, can help maintain their independence while ensuring their safety.
Difficulty with Visual Perception
Visual perception refers to the brain's ability to interpret and make sense of visual information received from the eyes. In Alzheimer's disease, individuals may experience difficulties with visual perception, leading to problems with depth perception, object recognition, and distinguishing colors or contrasts. These challenges can impact their ability to perform daily tasks effectively and safely.
Caregivers can provide support by creating an environment that is visually clear and organized. This can involve reducing clutter, using contrasting colors to enhance visibility, and ensuring adequate lighting in different areas of the living space. Additionally, it may be helpful to use visual cues or labels to assist with object recognition and navigation.
Understanding the impact of vision changes in Alzheimer's disease is crucial for caregivers to provide appropriate care and support. Regular eye exams can also be beneficial in detecting any ocular abnormalities associated with Alzheimer's. By addressing vision-related challenges and making necessary adjustments, caregivers can contribute to enhancing the quality of life for individuals with Alzheimer's disease.
Ocular Biomarkers for Alzheimer's
In recent years, researchers have been exploring the potential of the eye as a window into the early detection of Alzheimer's disease. The eye offers itself as a transparent medium to cerebral pathology and has potentiated the development of ocular biomarkers for Alzheimer's disease, enabling earlier diagnosis in the clinical setting and potentially improving disease management and quality of life for patients.
Role of the Eye in Early Diagnosis
The eye plays a vital role in the early diagnosis of Alzheimer's disease. Several studies have focused on identifying changes in the eye that may serve as potential biomarkers for early detection. Retinal changes observed in animal models of Alzheimer's disease, for example, include the accumulation of amyloid β peptides and evidence of retinal ganglion cell apoptosis. These findings provide valuable insights into the disease pathology and offer potential biomarkers for diagnosis [2].
Researchers have also found promising results in tears as a unique source of biomarkers for Alzheimer's disease detection. Tears contain amyloid β (Aβ) and tau proteins, and studies have shown elevated levels of total tau (t-tau) and Aβ peptide 42 (Aβ42) in tears of AD patients. This suggests that tears could serve as a non-invasive and accessible method for early detection.
Changes in Retinal Structures
The retina, located at the back of the eye, has garnered particular attention in the search for ocular biomarkers for Alzheimer's disease. Corneal nerve fiber length, density, and branch density have been identified as potential structural biomarkers for detecting early Alzheimer's disease. Studies have reported morphological differences in corneal nerve fibers of AD patients compared to healthy controls, providing further evidence of the potential of the eye in early diagnosis [3].
Furthermore, research has explored the presence of biomarkers related to Alzheimer's disease in ocular fluids such as aqueous humor (AH) and vitreous humor (VH). Significant levels of soluble APP (sAPP), Aβ40, Aβ42, total tau (t-tau), and neurofilament light chain (NfL) have been detected in AH and VH. Concentrations of these biomarkers in VH were associated with lower cognitive function, suggesting a potential link between ocular fluid biomarkers and AD severity.
While further research is needed to validate and refine these ocular biomarkers, the early findings are promising. The eye's potential to provide non-invasive and accessible means for early Alzheimer's disease detection could revolutionize diagnosis and improve outcomes for individuals at risk.
Understanding the role of the eye in early diagnosis and the changes observed in retinal structures brings us one step closer to developing effective screening methods for Alzheimer's disease. Continued research in this area holds the potential to transform the way we detect, manage, and treat this debilitating condition.
Eye-Related Symptoms in Alzheimer's
As Alzheimer's disease (AD) progresses, it can manifest in various eye-related symptoms that may provide early indications of the condition. Understanding these symptoms can be helpful in identifying potential cognitive decline. Here, we will explore two common eye-related symptoms associated with Alzheimer's: impaired visual recognition and ocular pathologies.
Impaired Visual Recognition
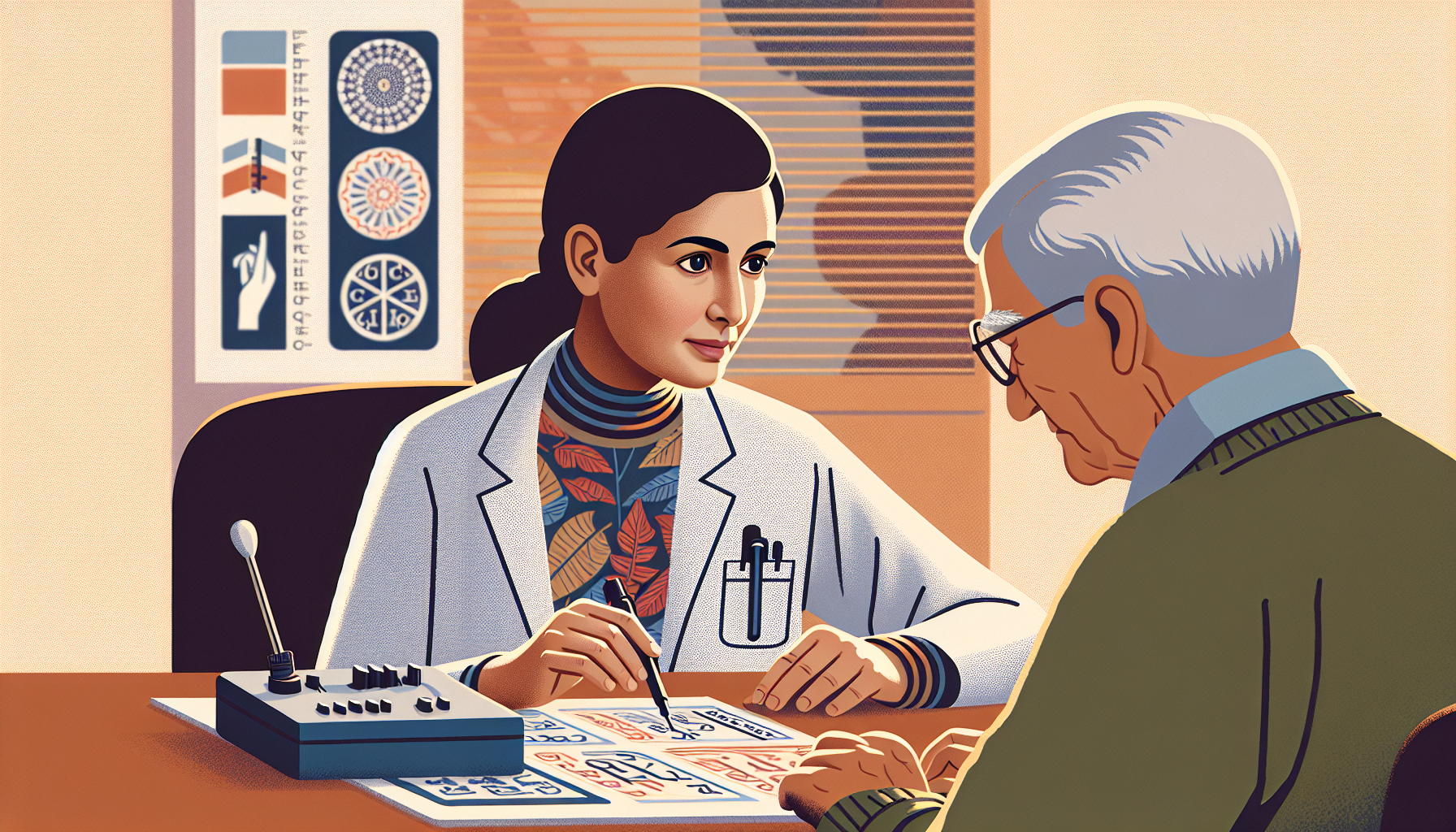
Studies have shown that patients with AD often experience impaired visual recognition, which can manifest in different ways. They may have difficulty describing complex photographs, recognizing figures from unusual perspectives, identifying incomplete letters, or recognizing familiar faces. In advanced stages of AD, individuals may also exhibit visual apperceptive agnosia, spatial recognition difficulties, and impaired vision-hand coordination.
These visual recognition challenges can be particularly noticeable to caregivers and loved ones, as individuals with AD may struggle to identify and interact with objects or people they once recognized easily. If you observe such symptoms in someone you care for, it may be worth consulting a healthcare professional to evaluate their cognitive health.
Ocular Pathologies and Cognitive Decline
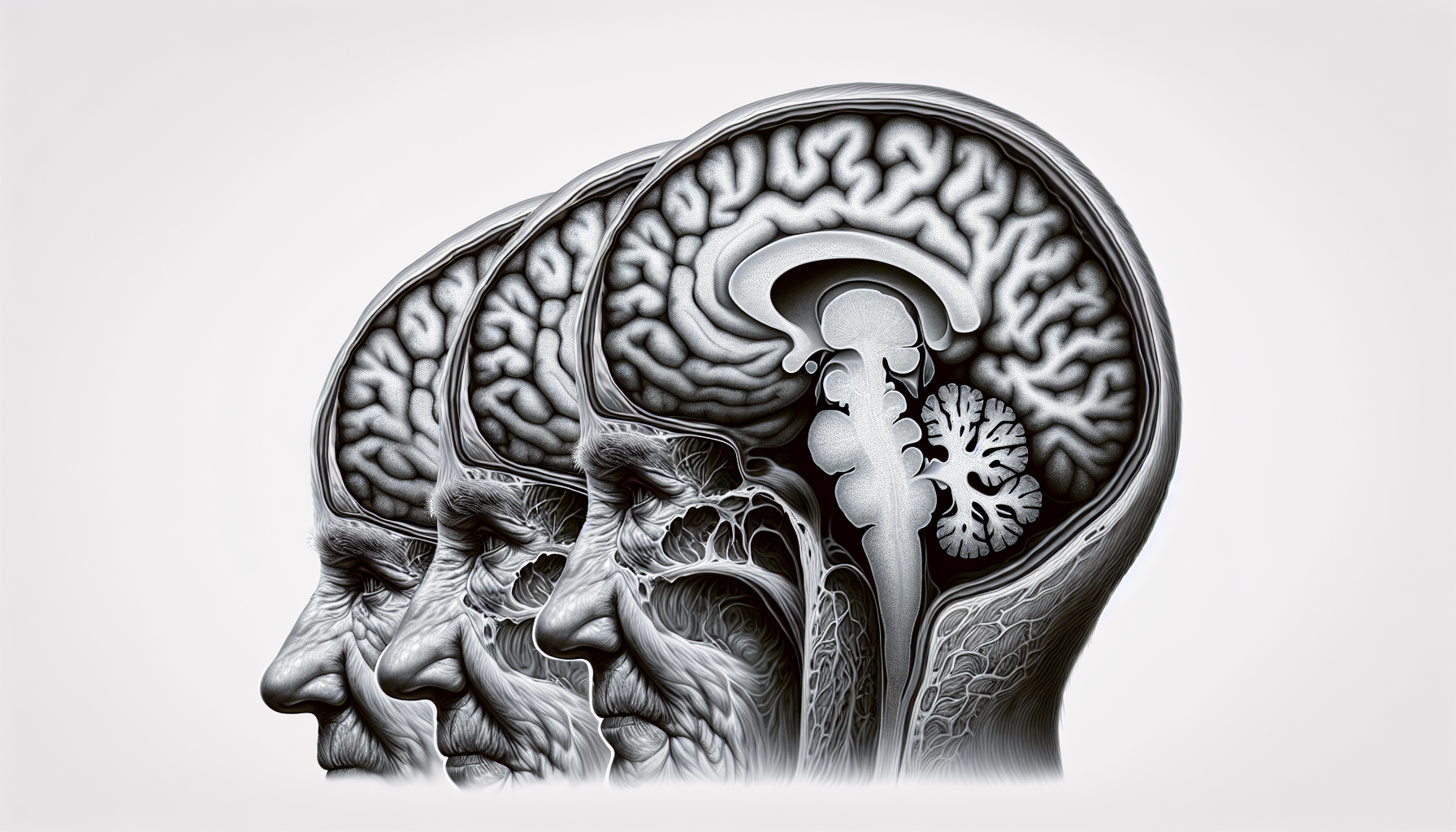
Recent research has discovered a correlation between ocular pathologies and cognitive decline in AD. Changes in the retina of patients with mild cognitive impairment and Alzheimer's disease have been found to correspond with changes in specific brain regions associated with memory, navigation, and time perception, such as the entorhinal and temporal cortices. These changes in the retina have been observed even in patients who appear cognitively normal or mildly impaired, suggesting a potential early predictor of later cognitive decline.
Furthermore, studies have revealed the accumulation of highly toxic proteins in the retinas of patients with Alzheimer's disease and mild cognitive impairment. This accumulation leads to severe degeneration of retinal cells, further supporting the link between ocular pathologies and cognitive decline.
These findings highlight the potential use of ocular biomarkers, such as changes in the retina, as a means of early detection and prediction of cognitive decline in AD. However, it's important to note that further research is needed to fully understand the relationship between ocular pathologies and Alzheimer's disease.
By being aware of impaired visual recognition and ocular pathologies, caregivers and healthcare professionals can monitor individuals for potential early signs of Alzheimer's disease. Regular eye examinations may prove valuable in detecting these changes and providing insights into cognitive health.
Ocular Imaging for Alzheimer's
In the quest to better understand and detect Alzheimer's disease in its early stages, ocular imaging has emerged as a promising tool. Two types of ocular imaging techniques that have shown potential in this area are CT imaging for ocular trauma and retinal imaging.
CT Imaging for Ocular Trauma
CT (computed tomography) imaging plays a crucial role in evaluating ocular trauma. It allows for three-dimensional visualization of the orbital bones, soft tissues, and ocular structures, making it an essential diagnostic modality for assessing a wide range of trauma-related pathologies. CT is particularly effective in detecting fractures of the orbital bones, with the medial and inferior walls being the most susceptible to fracture [6]. In cases of ocular or orbital foreign bodies, CT can accurately identify and characterize these objects, aiding in treatment planning.
Potential of Retinal Imaging
Retinal imaging has shown promise in detecting early signs of Alzheimer's disease. Research suggests that retinal imaging can identify amyloid beta plaques in the retina and retinal vessels, indicating changes in the cerebral vasculature associated with the early stages of neurodegenerative diseases. This non-invasive imaging technique holds potential as a tool for early detection and monitoring of Alzheimer's disease, providing valuable insights into the pathophysiological changes occurring in the brain.
By examining the retina and retinal vessels through specialized imaging techniques, researchers hope to gain further understanding of the relationship between ocular changes and neurodegenerative diseases like Alzheimer's. This may lead to the development of new diagnostic methods and treatment approaches in the future.
While ocular imaging techniques like CT and retinal imaging show promise in the context of Alzheimer's disease, further research and validation are needed to establish their clinical utility. However, these advancements in ocular imaging provide hope for the early detection and management of Alzheimer's disease, potentially improving outcomes for individuals affected by this debilitating condition.
Eye Exams for Detecting Health Conditions
Regular eye exams are not only important for maintaining good eye health but can also provide valuable insights into your overall health. Eye-related signs and symptoms observed during an eye examination can be indicative of various systemic diseases. It is essential to recognize these signs early on as they can contribute to the early detection and management of these conditions.
Eye-Related Signs of Systemic Diseases
During an eye exam, certain signs can point to underlying systemic diseases. Here are some examples:
- Diabetes: An eye exam can detect early signs of diabetes by observing changes in the blood vessels of the retina. Leaking yellow fluid or blood from tiny blood vessels may indicate diabetic retinopathy. In some cases, these changes may be present even before an individual has been diagnosed with diabetes, emphasizing the importance of early detection to prevent vision loss and other complications.
- Heart Disease: Careful examination of the retina using optical coherence tomography during an eye exam can reveal microscopic marks indicative of an eye stroke, which are found in higher numbers in individuals with heart disease. These findings suggest a link between eye health and cardiovascular health.
- High Blood Pressure: Unusual bends, kinks, or bleeding from blood vessels in the back of the eye can be observed during a dilated eye exam. These signs may indicate high blood pressure, which is a known risk factor for various eye diseases such as glaucoma, diabetic retinopathy, and macular degeneration.
- High Cholesterol: Presence of a yellow or blue ring around the cornea, especially in individuals younger than 40 years old, can be an indication of high cholesterol levels. Additionally, deposits in the blood vessels of the retina may also suggest elevated cholesterol levels, which could be a precursor to a life-threatening stroke [7].
- Stroke: An eye exam can sometimes reveal signs of an increased risk for a stroke. Blockages or clots in the blood vessels of the retina can lead to sudden blind spots or a sensation of a "curtain" closing over one's vision. Recognizing these signs during an eye exam can prompt further investigation and monitoring for vascular issues.
Importance of Regular Eye Exams
Regular eye exams play a vital role in detecting not just eye-related conditions but also systemic diseases. By monitoring the health of your eyes, an eye care professional can identify potential signs and symptoms that may warrant further investigation or medical attention. Detecting these conditions early can lead to timely intervention, better management, and improved overall health outcomes.
It is recommended to schedule regular comprehensive eye exams, especially if you have a family history of certain diseases or if you have risk factors associated with these conditions. By prioritizing regular eye exams, you can take a proactive stance toward your health and potentially identify underlying systemic diseases at an earlier stage.
Remember, your eyes can provide valuable insights into your overall well-being, so don't neglect the importance of regular eye exams. Consult with your eye care professional to determine the frequency of exams based on your specific needs and risk factors.
References
[1]: https://www.alz.org/alzheimers-dementia/10_signs
[2]: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4836138/
[3]: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10444735/
[4]: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8910735/
[5]: https://www.cedars-sinai.org/newsroom/new-insights-eye-damage-in-alzheimers-disease-patients/
[6]: https://www.ncbi.nlm.nih.gov/books/NBK572102/
[7]: https://www.aao.org/eye-health/tips-prevention/surprising-health-conditions-eye-exam-detects