Best Pain Medication For Elderly Patients
Discover the best pain medication for elderly patients!

Understanding Elderly Pain
As individuals age, the prevalence of pain becomes more common and can have a significant impact on their quality of life. Understanding the prevalence of pain in the elderly population and its impact is crucial for caregivers in providing appropriate care and support.
Prevalence of Pain in Elderly
Pain is a significant problem in older adults, with a high prevalence among the elderly population. In fact, studies have shown that the prevalence of pain in patients over 60 years old is more than twice that reported for patients under 60 years old. Around 60% of independent elderly patients and 80% of long-term care geriatric patients report substantial daily pain, making it one of the most common symptoms reported by elderly patients.

The prevalence of chronic pain in older adults can vary across different countries. For example, about 30% of Canadian older adults report pain, while rates in European countries range from about 19% in Switzerland to 46% in France [2]. Similar prevalence rates have been reported in other countries, such as Iran (32%) and China (41%).
Impact of Pain on Quality of Life
Pain in older adults can have a profound impact on their quality of life. Chronic pain, particularly persistent pain associated with musculoskeletal conditions and multimorbidity, is a particularly common issue among the elderly population. It is associated with significant disability, reduced mobility, sleep disturbances, depression, anxiety, and increased healthcare utilization [2].
Older adults with a combination of pain and depression are particularly vulnerable to physical disability, and chronic pain has been strongly linked to excess disability, insomnia, depression, and increased healthcare utilization. Additionally, chronic pain can disrupt familial and social relationships, further impacting the overall well-being of elderly individuals.
By understanding the prevalence of pain in the elderly population and the impact it has on their quality of life, caregivers can better recognize the importance of addressing pain management and providing appropriate care for elderly individuals.
Medication Options for Elderly Pain
When it comes to managing pain in elderly patients, there are several medication options available. It's important to consider the individual needs and health conditions of the patient when selecting the appropriate pain medication. Here are three commonly used medication options for elderly pain management:
Acetaminophen as Front-line Therapy
Acetaminophen is often recommended as the first-line therapy for treating pain in the geriatric population [1]. It is a safe and effective option for mild to moderate chronic pain in elderly patients, with a favorable safety profile. Acetaminophen selectively inhibits prostaglandin synthesis in the central nervous system, providing pain relief [1].
The maximum daily dosage of acetaminophen is 4 grams, and dose adjustments may be necessary for patients with hepatic dysfunction. It is important to note that many common over-the-counter medications contain acetaminophen, so patients should carefully examine all formulations to avoid exceeding the recommended dosage [1]. Acetaminophen is generally well tolerated by elderly patients, including those over 65 years of age.
Caution with Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
Nonsteroidal anti-inflammatory drugs (NSAIDs) are another option for managing pain in elderly patients, particularly for mild to moderate musculoskeletal pain and inflammation. However, caution is advised when using NSAIDs due to their potential side effects [4]. It is recommended to use the lowest effective dose for the shortest duration to minimize adverse events.
Topical NSAIDs containing diclofenac, ibuprofen, or ketoprofen have shown the best evidence for both acute and chronic conditions. These topical formulations are generally well tolerated and suitable for patients over 65 years of age.
Opioids for Severe Pain
In cases of severe pain that is not adequately controlled with other medications, opioids may be prescribed for elderly patients. However, the use of opioids in the elderly population requires careful consideration due to multiple comorbidities and the risk of polypharmacy.
Determining the appropriate opioid drug, dosage, and maintenance of therapy can be challenging in elderly patients. Close monitoring and regular reassessment of the patient's pain levels and response to treatment are essential. Dosing adjustments may be necessary to ensure optimal pain management and minimize the risk of adverse effects.
It's crucial to consult with a healthcare professional to determine the most suitable pain medication for an elderly patient. The medication choice should be based on the individual's pain severity, medical history, and potential interactions with other medications. Regular communication between the caregiver, patient, and healthcare team is vital to ensure effective pain management and the overall well-being of the elderly patient.
Special Considerations for Elderly Patients
When it comes to managing pain in elderly patients, there are several special considerations that need to be taken into account. These considerations include dosing adjustments for opioids, potential side effects and risks, as well as pharmacological limitations.
Dosing Adjustments for Opioids
Opioids have been recognized as effective in treating non-cancer chronic pain in the elderly population, but they are often underutilized. It's important to note that geriatric patients may require initially reduced doses of opioids, typically around 50% less compared to younger patients. This adjustment helps to minimize the risk of adverse effects while still providing effective pain relief.
Side Effects and Risks
While opioids can provide significant pain relief, it's essential to be aware of the potential side effects and risks, especially in elderly patients. Common side effects of opioids in this population include nausea, constipation, urinary retention, central nervous system adverse effects (such as sedation, cognitive impairment, and myoclonus), pruritus, respiratory depression, opioid-induced hyperalgesia, cardiovascular effects (such as QT prolongation), and endocrine effects (such as reduced serum luteinizing hormone and cortisol levels, and increased prolactin levels) [5].
To manage these side effects, it may be necessary to reduce the opioid dose, add adjuvant therapy, or closely monitor the patient's response. Careful consideration should be given to the risks and benefits of opioid therapy, and the treatment plan should be individualized to meet the specific needs of each patient.
Pharmacological Limitations
In addition to dosing adjustments and potential side effects, it's important to be aware of the pharmacological limitations of pain medications in elderly patients. For example, nonsteroidal anti-inflammatory drugs (NSAIDs) should be used with caution in this population due to the increased risk of complications such as renal failure, gastropathy, and cardiovascular disease. Geriatric patients are more susceptible to these adverse effects, and therefore alternative pain management strategies may need to be considered.
Acetaminophen represents a front-line therapy for treating pain in the geriatric population. However, it's important for patients to examine all over-the-counter medications, as many formulations contain acetaminophen. This selective inhibition of prostaglandin in the central nervous system can help alleviate pain.
Understanding and addressing these special considerations for elderly patients is crucial for safe and effective pain management. Working closely with healthcare professionals and considering a multimodal approach that combines pharmacological and non-pharmacological strategies can help optimize pain relief while minimizing risks and adverse effects.
Non-Pharmacological Approaches
In addition to medication options, non-pharmacological approaches play a significant role in managing pain in elderly patients. These approaches focus on addressing pain through techniques that do not involve medications. Here are three non-pharmacological approaches that have shown promise in managing pain in older adults:
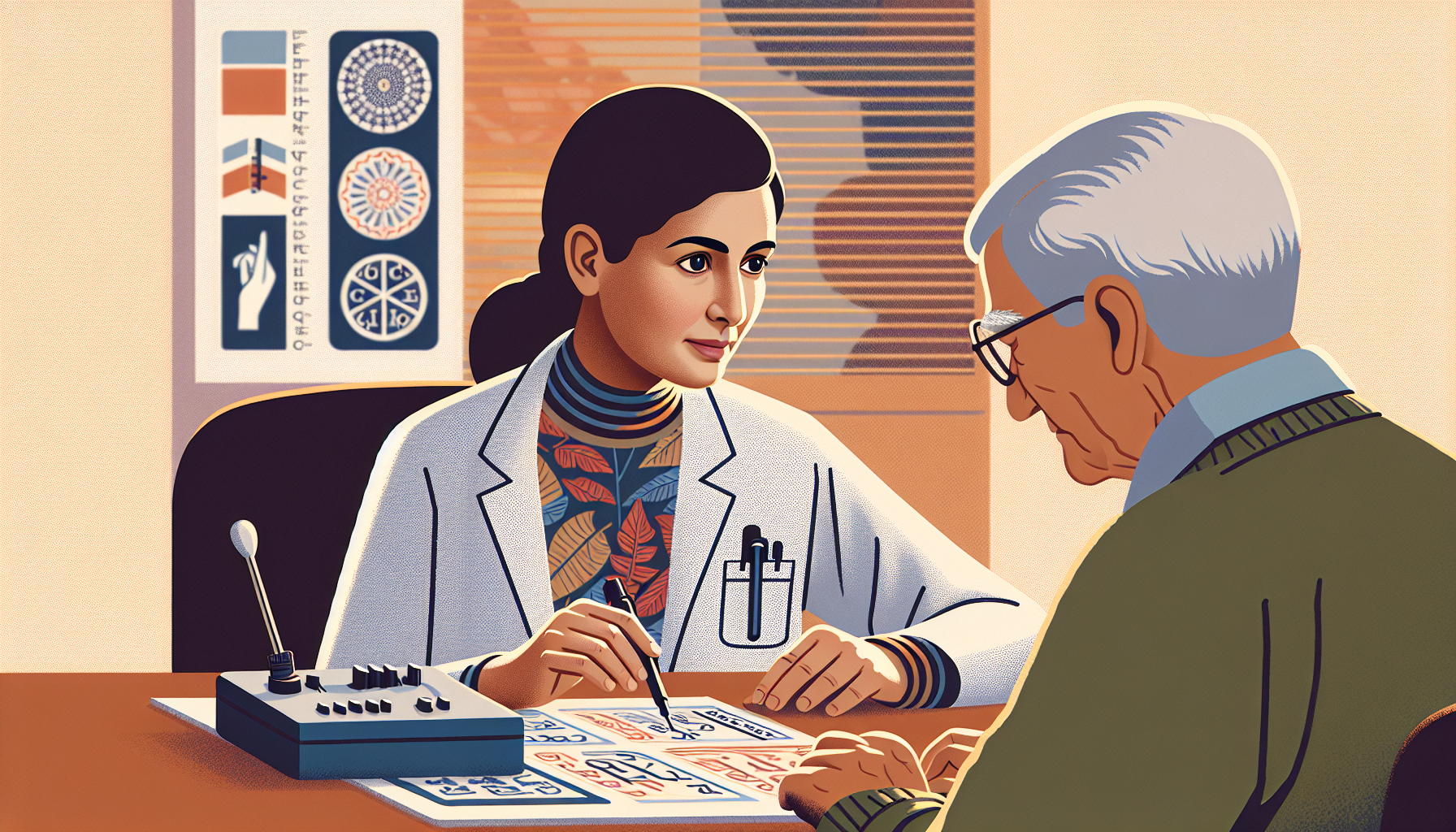
Cognitive Behavioral Therapy
Cognitive-behavioral therapy (CBT) has been found to be beneficial for older adults in managing chronic pain. Studies have shown that older adults can obtain equal benefits from CBT pain interventions compared to younger adults. CBT focuses on identifying and re-framing negative thoughts and beliefs related to pain, as well as learning techniques to manage pain-related symptoms and improve overall well-being.
During CBT sessions, individuals work with a therapist to develop coping strategies, relaxation techniques, and problem-solving skills. By addressing the psychological and emotional aspects of pain, CBT can help older patients better manage their pain and enhance their quality of life.
Progressive Relaxation Techniques
Progressive relaxation techniques involve systematically tensing and then relaxing different muscle groups in the body. This approach aims to reduce muscle tension and promote overall relaxation, thereby alleviating pain. Older patients can benefit from practicing progressive relaxation techniques as part of their pain management strategy.
By practicing progressive relaxation regularly, individuals can learn to recognize and release muscle tension, which may contribute to pain. This technique can be performed independently or with the guidance of a therapist or through instructional videos or apps. It offers a simple and accessible way for older adults to manage pain and promote relaxation.
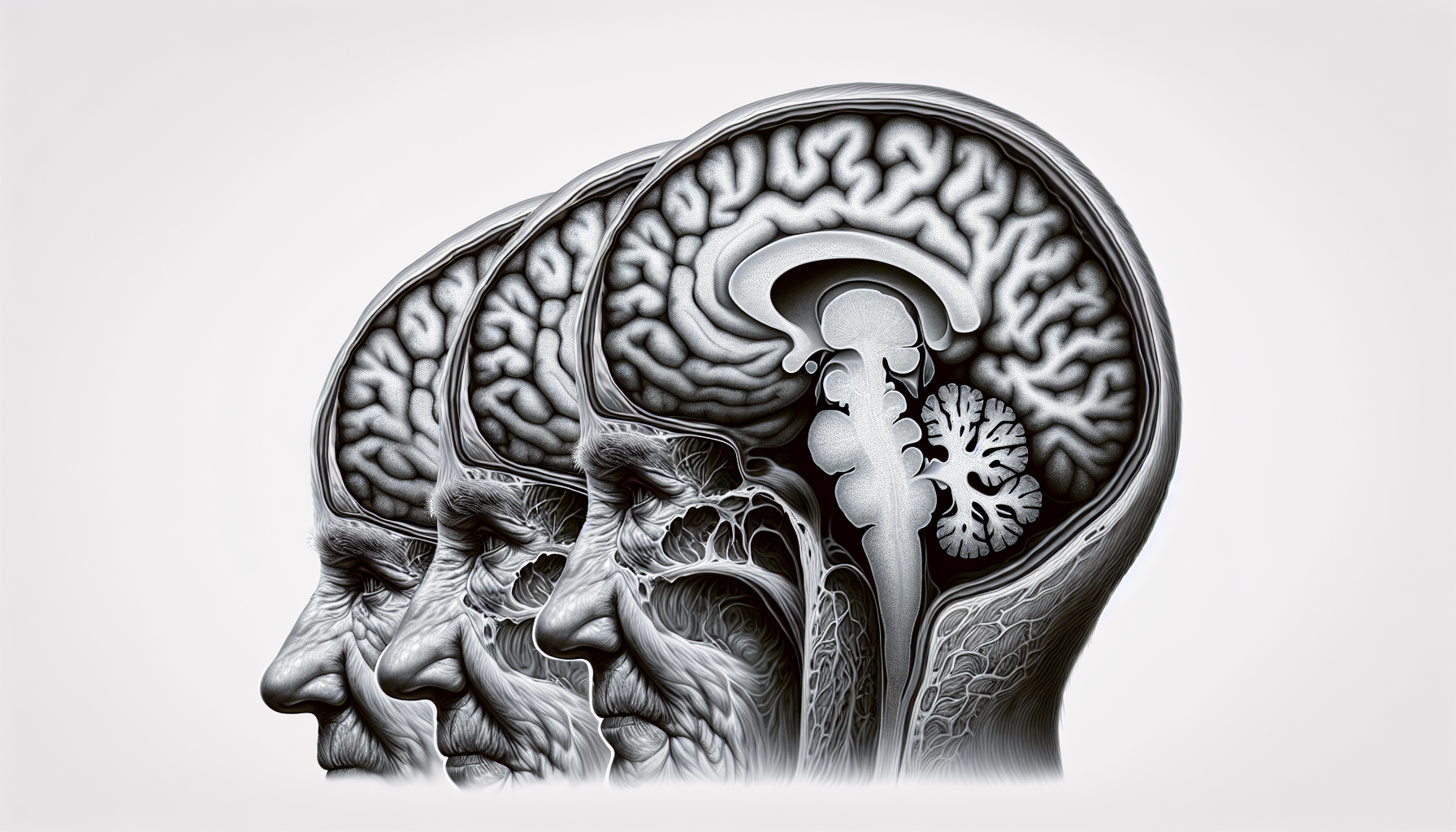
Pain Neuroscience Education
Pain neuroscience education is an approach that focuses on educating individuals about the complex nature of pain and how it is processed by the brain. By understanding the mechanisms behind pain, individuals can develop a different perspective on their pain experience, reducing fear and anxiety associated with pain.
Pain neuroscience education helps older patients reframe their understanding of pain and empowers them to take an active role in managing their pain. It involves explaining the biology of pain, the role of the nervous system, and the factors that can influence pain perception. This approach can be delivered through individual or group sessions with healthcare professionals specializing in pain management.
By incorporating these non-pharmacological approaches into the pain management plan for elderly patients, caregivers can provide additional tools and strategies to help alleviate pain and improve overall well-being. It's important to remember that each individual may respond differently to these techniques, so a personalized approach is key.
Chronic Pain Management Guidelines
When it comes to managing chronic pain in elderly patients, it's important to follow established guidelines to ensure safe and effective treatment. The American Geriatrics Society (AGS) has provided recommendations that can serve as a valuable resource for caregivers and healthcare professionals.
American Geriatrics Society Recommendations
The AGS 2002 Guidelines for the Management of Persistent Pain in Older Adults offer valuable insights for chronic pain management in elderly patients. These recommendations emphasize the need to simplify pain regimens and avoid polypharmacy. By simplifying the medication regimen, caregivers can minimize the risk of medication interactions and adverse effects.
The guidelines also suggest starting medications at lower dosages, titrating upward as needed. Age-associated changes in pharmacokinetics and pharmacodynamics necessitate starting opioids at lower doses (approximately 25%-50% of the dose given to younger patients) in the elderly. Careful monitoring and adjustment of opioid dosages is crucial to ensure optimal pain relief while minimizing the risk of side effects.
Avoiding Polypharmacy
Polypharmacy, the simultaneous use of multiple medications, is a common concern in the elderly population. It can lead to increased medication-related problems and adverse effects. The AGS guidelines highlight the importance of avoiding polypharmacy in chronic pain management. By carefully evaluating the medication regimen and minimizing the number of medications, healthcare providers can reduce the risk of drug interactions and improve overall patient safety.
Individualized Treatment Approaches
Pain management in elderly patients should be approached on an individual basis. The AGS guidelines emphasize the need for personalized treatment plans that consider the unique characteristics and needs of each patient. This individualized approach allows healthcare providers to tailor pain management strategies to the specific circumstances of the patient, taking into account factors such as comorbidities, medication tolerability, and potential drug-drug interactions.
By following the recommendations set forth by the American Geriatrics Society, caregivers can ensure that elderly patients receive appropriate and safe pain management. It is essential to work closely with healthcare professionals to develop a comprehensive pain management plan that prioritizes the patient's comfort, quality of life, and overall well-being.
Addressing Pain in Geriatric Care
When it comes to addressing pain in geriatric care, a comprehensive approach is essential to ensure the well-being and comfort of elderly patients. This section will discuss three key components of addressing pain in geriatric care: multimodal pain management, comprehensive assessment strategies, and collaborative care approaches.
Multimodal Pain Management
Multimodal pain management involves utilizing a combination of different therapeutic interventions to effectively manage pain in elderly patients. It recognizes that pain is a complex and multidimensional experience that can be influenced by various factors. By employing multiple approaches simultaneously, healthcare providers can optimize pain relief while minimizing the potential risks and side effects associated with certain medications.
Multimodal pain management may include a combination of the following:
- Medications: Depending on the severity and type of pain, healthcare providers may prescribe analgesics such as opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), or acetaminophen. It is important to note that opioids, although effective in managing pain, should be used with caution and their dosage should be adjusted for elderly patients.
- Non-pharmacological interventions: These include physical therapy, occupational therapy, cognitive behavioral therapy, relaxation techniques, and pain neuroscience education. These approaches aim to address pain through methods that do not rely solely on medication.
- Complementary and alternative therapies: Some elderly patients find relief from pain through complementary therapies such as acupuncture, massage, or herbal remedies. However, it is crucial to consult with healthcare providers before incorporating these therapies into a pain management plan.
By combining various interventions, multimodal pain management provides a more holistic and individualized approach to pain relief in geriatric care.
Comprehensive Assessment Strategies
Comprehensive assessment strategies are crucial in accurately understanding and addressing pain in elderly patients. Pain can be a significant problem in older adults, with over half of the population aged 65 and older projected to have pain, particularly persistent pain associated with musculoskeletal conditions and multimorbidity.
To effectively assess pain in geriatric patients, healthcare providers should consider the following:
- Pain scales: Utilizing validated pain scales, such as the Numeric Rating Scale (NRS) or the Faces Pain Scale, can help quantify and monitor pain levels over time.
- Patient self-report: Encouraging open communication and actively listening to patients' descriptions of their pain is essential for a comprehensive assessment.
- Observational assessment: In cases where patients are unable to communicate their pain, healthcare providers can assess pain indicators through observation, such as facial expressions, body movements, and changes in behavior.
- Medical history and physical examination: Understanding the patient's medical history, including any underlying conditions or previous pain management approaches, can provide valuable insights for a comprehensive assessment.
By employing comprehensive assessment strategies, healthcare providers can obtain a clearer understanding of the nature and intensity of pain experienced by geriatric patients. This knowledge is crucial for developing effective pain management plans.
Collaborative Care Approaches
Collaborative care approaches involve a team-based approach to pain management, ensuring that healthcare professionals work together to address the unique needs of geriatric patients. This collaborative effort may involve primary care physicians, pain specialists, physical therapists, occupational therapists, pharmacists, and other healthcare professionals.
Key elements of collaborative care approaches in geriatric pain management include:
- Interdisciplinary communication: Regular communication and information sharing among healthcare providers involved in the patient's care are essential for comprehensive pain management.
- Care coordination: Coordinating care between different healthcare professionals can help ensure that all aspects of pain management are addressed and that treatments are aligned.
- Patient and caregiver involvement: Engaging patients and their caregivers in the decision-making process and providing education about pain management strategies can improve treatment outcomes and patient satisfaction.
By fostering collaboration among healthcare providers and involving patients and their caregivers in the care process, geriatric pain management can be more effective and patient-centered.
Addressing pain in geriatric care requires a multimodal approach, comprehensive assessment strategies, and collaborative care approaches. By implementing these components, healthcare providers can tailor pain management plans to the unique needs of elderly patients, improving their overall quality of life and well-being.
References
[1]: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6173536/
[2]: https://www.sciencedirect.com/topics/medicine-and-dentistry/pain-in-older-adult
[3]: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6235641/
[4]: https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/