Experimental Treatments In Home Care
Discover the potential of experimental treatments in home care for enhanced wellness and care.

Lifestyle Management in Concierge Home Care
In concierge home care, lifestyle management plays a crucial role in ensuring the well-being and comfort of senior patients. This approach focuses on providing personalized care and support tailored to meet individual needs. Three key components of lifestyle management in concierge home care are personalized nutrition plans, assistance with daily activities, and intravenous (IV) therapy at home.
Personalized Nutrition Plans
Dietitians work closely with patients to develop personalized nutrition plans that align with their health goals and specific dietary needs. These plans take into account various health conditions such as diabetes, heart disease, cancer, and more. By working alongside healthcare professionals, dietitians monitor the progress of patients and provide ongoing guidance on managing nutrition-related concerns. They also educate patients on the importance of proper nutrition and how it can positively impact their overall health.

Benefits of Personalized Nutrition Plans
- Customized to individual dietary needs
- Helps manage specific health conditions
- Supports overall health and well-being
Assistance with Daily Activities
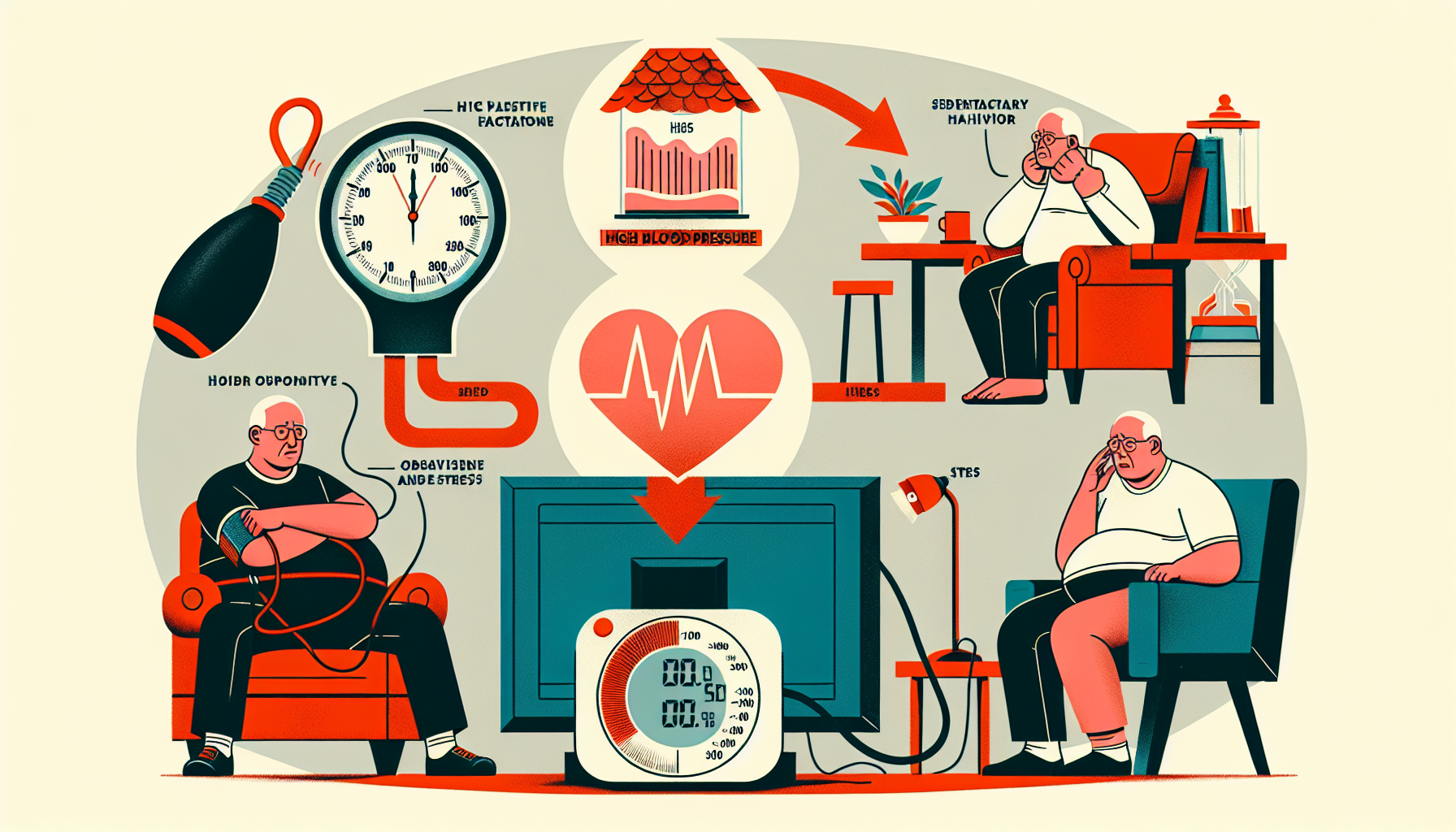
In concierge home care, personal support services are provided to assist individuals with daily activities. These services include grooming, dressing, bathing, medication compliance, wound dressings, and monitoring blood sugar and blood pressure. By providing support in these areas, caregivers help individuals maintain their independence and dignity while dealing with the challenges of aging, injury, or illness.
Personal Support Services
- Assistance with grooming, dressing, and bathing
- Medication compliance and monitoring
- Wound dressings and care
- Blood sugar and blood pressure monitoring
Telehealth Applications in Home Care
In the realm of home care, telehealth applications have become invaluable tools for managing various aspects of healthcare. These applications offer a platform to support disease management for home care patients diagnosed with chronic conditions and their families. They provide innovative solutions that bridge the gap between patients and healthcare providers, ensuring comprehensive care from the comfort of home.
Disease Management Support
Telehealth applications play a crucial role in disease management for home care patients. They offer continuous individualized help, web-based questionnaires, and data transmission to healthcare providers. With the use of these applications, patients diagnosed with chronic conditions such as asthma and diabetes can receive personalized support and monitoring in their home environment.
For example, home asthma telemonitoring systems utilize telehealth applications to assist in managing asthma symptoms. These systems enable patients to monitor their asthma symptoms, track medication usage, and transmit data to healthcare providers. By closely monitoring their condition with the help of these applications, patients can receive timely intervention and adjustments to their treatment plans, leading to better disease management outcomes.
Similarly, web-based tools for diabetes self-management have revolutionized home care for individuals with diabetes. Patients can utilize these tools to track their blood glucose levels, record their food intake, and monitor their physical activity. The data collected can be shared with healthcare providers, who can then provide targeted advice and make informed decisions regarding the patient's treatment plan. This level of personalized support empowers patients to actively participate in their own care and improve their overall well-being.
Innovative Telehealth Projects
Numerous innovative telehealth projects have been developed to enhance home care for patients with a range of conditions. These projects leverage technology to provide convenient access to healthcare services, monitor vital signs, and facilitate communication between patients and healthcare providers.
One such project is the Telematic Management of Insulin-Dependent Diabetes Mellitus, funded by the European Union. This project implemented a distributed computer-based system that allowed patients to download monitoring data from blood glucose monitoring devices and transmit them to the hospital information system.
This enabled physicians to remotely review the data and provide therapeutic advice to patients, ensuring optimal management of their diabetes.
Another notable project is the TeleHomeCare project at the University of Minnesota. This project focused on patients diagnosed with congestive heart failure, chronic obstructive pulmonary disease, or those requiring wound care. It utilized a system based on low-cost monitoring devices and an Internet application.
The system incorporated daily questionnaires, alerts for immediate clinical attention, and customization based on individual patient needs. By leveraging telehealth technology, patients received close monitoring and timely interventions, resulting in improved outcomes and reduced hospitalizations.
These innovative telehealth projects highlight the potential of technology to revolutionize home care. By embracing telehealth applications, caregivers and patients can access a wide range of services, receive timely support, and improve overall health outcomes. It is an exciting frontier in healthcare that empowers individuals to actively participate in their own care and promotes better overall well-being.
Experimental Treatments in Home Care
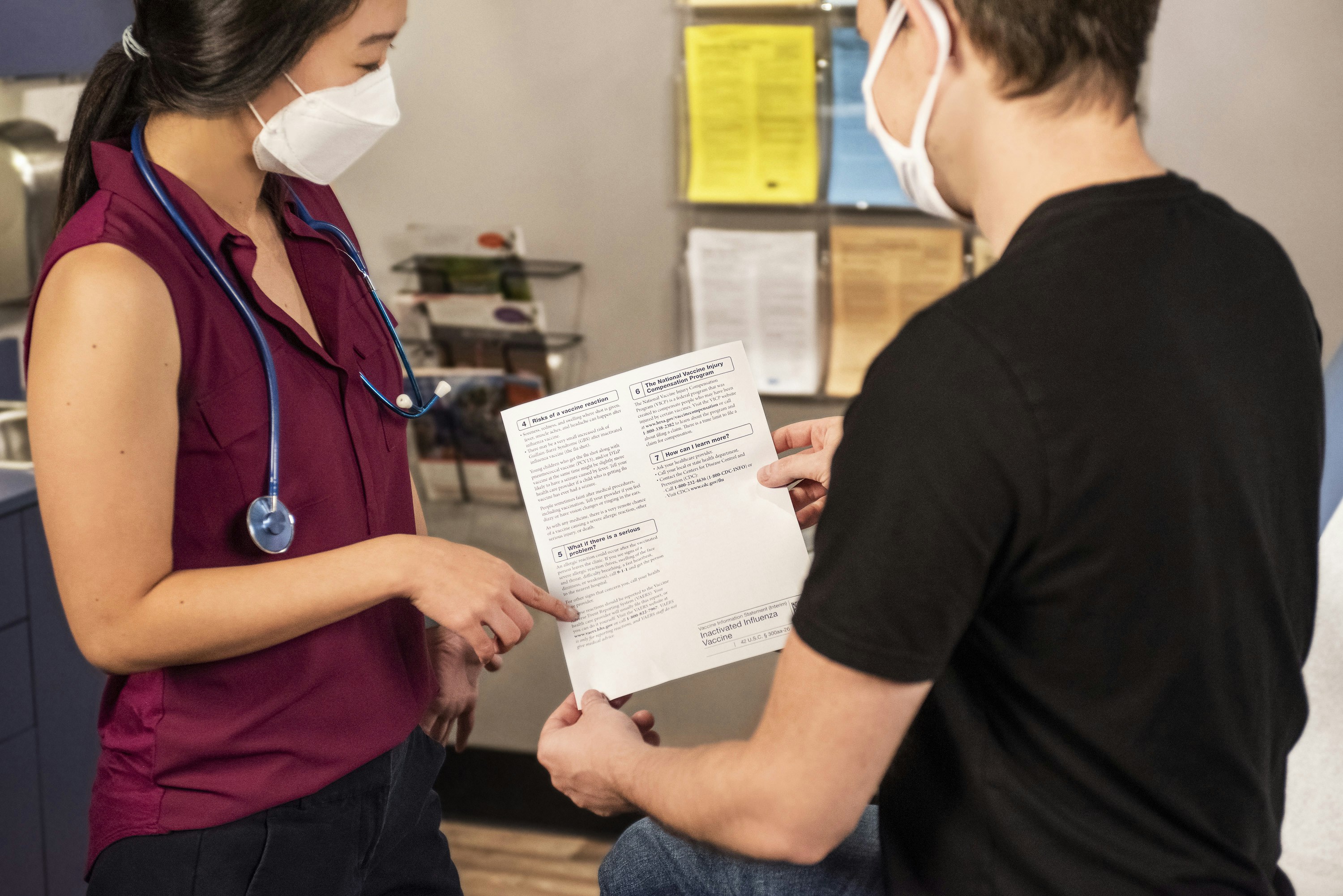
When it comes to home care, there are instances where experimental treatments may be explored as a potential option for patients. These treatments often involve participation in clinical trials and studies, which aim to assess the safety and effectiveness of new interventions. It's important to understand the benefits and risks associated with experimental treatments in home care.
Clinical Trials and Studies
Clinical trials and studies play a vital role in the development of new medications, surgical techniques, and behavioral interventions. These trials are designed to test the safety and efficacy of innovative treatments or prevention strategies, such as new drugs, diets, or medical devices [3]. By participating in clinical trials, patients have the opportunity to contribute to medical advancements and potentially receive cutting-edge care.
Before a clinical trial is conducted in humans, extensive laboratory tests and studies are performed in animals to evaluate the safety and efficacy of the potential intervention. If these preliminary studies demonstrate promising results, the U.S. Food and Drug Administration (FDA) grants approval for the intervention to be tested in humans [3].
Clinical trials progress through different phases, including Phase 1, 2, and 3, to assess safety, effectiveness, and potential side effects. In Phase 1, the focus is on determining the appropriate dosage and evaluating any adverse effects. Phase 2 involves a larger sample size to gather more data on safety and efficacy. Finally, in Phase 3, the intervention is tested on a larger population to confirm effectiveness and monitor potential side effects. If the intervention proves to be safe and effective, the FDA approves it for clinical use, while continuing to monitor its effects.
Participation in clinical trials and studies is essential, as diverse participants of varying ages, sexes, races, and ethnicities contribute to a better understanding of how new treatments and interventions work for different populations. It is through these trials that researchers can gain insight into the unique health needs and reactions to treatments among older adults.
Experimental Treatment Risks
While experimental treatments hold promise for the future of medical advancements, it's crucial to acknowledge the potential risks associated with these interventions. Since experimental treatments are still being tested, there is a level of uncertainty regarding their safety and effectiveness. The side effects and long-term outcomes of these treatments may not be fully understood.
It's important for patients and their caregivers to carefully consider the potential risks and benefits of participating in experimental treatments. Open communication with healthcare providers and researchers is essential to fully understand the nature of the treatment, the potential risks involved, and the expected outcomes.
Informed consent is a crucial aspect of participating in experimental treatments. Patients should be provided with detailed information about the treatment, including the purpose, procedures, potential risks and benefits, and alternative options. This enables patients and their caregivers to make well-informed decisions based on their unique circumstances and preferences.
Remember, experimental treatments are not suitable for everyone, and participation is entirely voluntary. It's important to consult with healthcare professionals, ask questions, and carefully evaluate the potential risks and benefits before deciding to participate in any experimental treatment in the home care setting.
Medication Management in Home Care
Ensuring proper medication management is a crucial aspect of home care, especially for elderly patients who often take multiple medications for various comorbidities. Addressing medication issues and providing effective wound care are essential components of home health services.
Addressing Medication Issues
According to a study, nearly one-third of older home health care patients face potential medication problems or are taking drugs considered inappropriate for older individuals. Many elderly patients receive prescriptions from multiple providers, resulting in the use of more than five prescription drugs simultaneously. This complexity increases the risk of medication errors and adverse reactions.
To address medication issues in home care, interventions have been tested and proven effective. Patient education delivered through telephone or videophone, followed by nurse support, has shown positive outcomes. Tailoring education to individual patients and promoting collaboration among providers (e.g., nurse, pharmacist, physician) have also been effective strategies.
Data from NCBI Bookshelf
Implementing these interventions as part of the home care plan can help reduce medication errors, improve medication adherence, and enhance patient safety.
Wound Care in Home Health
Wound care is another crucial aspect of home health services, as over a third of home health care patients require treatment for wounds. Additionally, nearly 42 percent of patients with wounds have multiple wounds. It is important to provide appropriate wound care to promote healing and prevent complications.
Home health care nurses play a vital role in wound care management. Studies have shown that most home health care nurses can accurately identify wound bed and periwound characteristics, ensuring appropriate treatment [4].
Interventions to improve wound care management in home health care have been tested and shown positive outcomes. When compared to traditional wet-to-dry or moist saline dressings, alternative wound treatments have demonstrated greater effectiveness and lower costs [4].
Table: Interventions to Improve Wound Care Management in Home Health Care
Data from NCBI Bookshelf
By implementing evidence-based wound care interventions, home health care providers can optimize healing, minimize complications, and improve overall patient outcomes.
Addressing medication issues and providing effective wound care are essential components of home care. By utilizing interventions that have shown positive outcomes, home health care providers can enhance medication management and promote optimal wound healing for their patients.
Health Monitoring in Home Care
In home care, health monitoring plays a crucial role in ensuring the well-being and safety of patients. Two key aspects of health monitoring in home care are fall prevention strategies and reducing unplanned hospital admissions.
Fall Prevention Strategies
Falls are a common concern among elderly individuals, and home health care providers need to be equipped with effective fall prevention strategies. By implementing a fall-prevention program and utilizing standardized tools, healthcare professionals can assess the risk factors for falls and develop targeted interventions to prevent fall-related injuries [4].
An interdisciplinary approach involving healthcare professionals, including nurses, physical therapists, and occupational therapists, can be effective in reducing the risk of falls. This collaborative effort allows for a comprehensive assessment of the patient's home environment, identification of potential hazards, and implementation of appropriate interventions to minimize fall risks.
It's important to educate both patients and caregivers on fall prevention techniques, such as exercise programs to improve strength and balance, proper footwear, and home modifications to create a safe living space. Regular communication and follow-up with healthcare professionals can ensure the ongoing effectiveness of fall prevention strategies.
Unplanned Hospital Admission Reduction
Reducing unplanned hospital admissions is a significant goal in home health care. Evidence suggests that specialized, coordinated, interdisciplinary care can have a positive impact on reducing unplanned hospital admissions in specific home health care populations [4]. By implementing targeted interventions and utilizing process-of-care analysis, healthcare providers can identify areas for improvement and develop strategies to minimize unplanned hospital admissions.
The Outcome and Assessment Information Set (OASIS) is a valuable tool that provides data to analyze outcomes and guide quality improvement efforts in home health care. By leveraging this framework of Outcomes-Based Quality Improvement (OBQI), healthcare providers can identify trends, assess the effectiveness of interventions, and make informed decisions to reduce unplanned hospital admissions.
An interdisciplinary approach is essential in addressing the complex needs of home health care patients. By working closely with family caregivers and collaborating with Advanced Practice Nurses (APNs) and other healthcare professionals, nurses can enhance their effectiveness in providing patient-centered care. This includes electronic communication, reminders of protocols, disease-specific educational materials, and leveraging the expertise of APNs as clinical resources for staff [4].
By prioritizing fall prevention strategies and implementing effective measures to reduce unplanned hospital admissions, home health care providers can ensure the safety and well-being of their patients while promoting a higher quality of care.
Supporting Family Caregivers
When it comes to home care, supporting family caregivers is a crucial component in ensuring the well-being of both the caregivers and the senior patients they are caring for. By enhancing caregiver support and promoting effective interdisciplinary care, the overall quality of home care can be significantly improved.
Enhancing Caregiver Support
Evidence suggests that working closely with and supporting family caregivers is essential for helping patients remain in their homes [4]. Caregivers play a vital role in providing physical, emotional, and social support to their loved ones. To enhance caregiver support, various strategies can be implemented:
- Electronic communication: Providing caregivers with tools such as mobile apps or online portals can facilitate communication with healthcare professionals, allowing for quick access to information and guidance.
- Reminders of protocols: Sending regular reminders to caregivers about medication schedules, therapy sessions, and other important aspects of care can help ensure that patients receive the necessary treatments on time.
- Disease-specific educational materials: Offering educational resources tailored to the specific conditions of the patients can empower caregivers with the knowledge and skills to provide effective care at home.
- Collaboration with Advanced Practice Nurse (APN) colleagues: Working together with APNs who serve as clinical experts can provide additional support and guidance to caregivers, ensuring they have access to specialized knowledge and expertise when needed.
By implementing these strategies, caregivers can feel supported and empowered in their role, leading to improved patient outcomes and overall satisfaction.
Effective Interdisciplinary Care
In addition to enhancing caregiver support, effective interdisciplinary care is crucial for providing comprehensive and well-coordinated home care. Interdisciplinary care involves collaboration and communication among different healthcare professionals involved in the patient's care, including nurses, doctors, therapists, and social workers. This collaborative approach ensures that all aspects of the patient's well-being are addressed.
Key components of effective interdisciplinary care in home care include:
- Regular team meetings: Healthcare professionals involved in the patient's care should regularly come together to discuss the patient's progress, address any challenges, and develop a cohesive care plan.
- Care coordination: By assigning a designated care coordinator, the communication and coordination among the healthcare team members can be streamlined, reducing the chances of miscommunication or gaps in care.
- Continuity of care: Ensuring that there is seamless continuity of care as patients transition between different healthcare settings, such as hospitals, clinics, and home care, is essential. This includes accurate and timely exchange of medical information and effective handoffs between healthcare professionals.
By fostering effective interdisciplinary care, caregivers can benefit from the expertise and collaboration of a diverse team, resulting in improved patient outcomes and a more positive care experience for both the caregivers and the patients.
Supporting family caregivers through enhanced support and effective interdisciplinary care is crucial in providing high-quality home care. By recognizing and addressing the needs of caregivers, the overall care experience can be more positive and impactful, ultimately leading to better outcomes for senior patients receiving care at home.
References
[1]: https://healthcareathome.ca/community-care/specialized-services/
[2]: https://www.ncbi.nlm.nih.gov/books/NBK210061/
[3]: https://www.nia.nih.gov/health/clinical-trials-and-studies/what-are-clinical-trials-and-studies/