Parkinson's Disease Dementia Stages
From cognitive changes to treatment options, we've got you covered!

Understanding Parkinson's Disease Dementia
Parkinson's disease dementia is a common complication that affects a significant percentage of individuals with Parkinson's disease. According to Healthline, an estimated 50 to 80 percent of people with Parkinson's will eventually experience Parkinson's disease dementia. Research has shown that dementia is present in about 83 percent of those still living with Parkinson's disease after 20 years. Additionally, up to 70 percent of people with Parkinson's may develop dementia as part of the disease progression, as per the Parkinson's Foundation.
Frequency and Progression
The development of Parkinson's disease dementia can vary from person to person. Some studies have reported that the average time from onset of Parkinson's to developing dementia is about 10 years. However, it's important to note that cognitive changes and the timing of their occurrence can differ among individuals with Parkinson's disease. Before developing dementia, individuals may experience milder cognitive changes known as mild cognitive impairment (MCI). Among those with normal cognition at Parkinson's diagnosis, around 30% will develop MCI after five years.

Impact on Lifespan
While people with Parkinson's disease can generally expect a similar lifespan to the general population, both Parkinson's disease dementia and Lewy body dementia can potentially shorten lifespan due to medical complications associated with the diseases. It's important to note that the medical complications, rather than the diseases themselves, are often the primary cause of the shorter lifespan.
Understanding the frequency and progression of Parkinson's disease dementia is crucial for caregivers and individuals with Parkinson's to effectively manage the condition and provide appropriate care. Regular communication with healthcare professionals and a supportive network can help individuals navigate the challenges associated with Parkinson's disease dementia and improve the overall quality of life.
Symptoms and Challenges
Parkinson's disease dementia (PD-D) can present a variety of symptoms that impact cognitive function and behavioral well-being. Understanding these symptoms is crucial for caregivers and patients alike. The two main categories of symptoms seen in PD-D are cognitive changes and behavioral and emotional symptoms.
Cognitive Changes
Cognitive changes are common in individuals with PD-D. These changes may include memory impairments, confusion, difficulties with problem-solving and abstract thinking, and challenges with attention and concentration. Speaking and communication may become more challenging, and individuals may experience trouble understanding and expressing themselves. Table 1 provides an overview of the cognitive symptoms associated with PD-D.
Cognitive Changes
- Memory impairments
- Confusion
- Problems with problem-solving and abstract thinking
- Difficulties with attention and concentration
- Challenges with speaking and communication
Table 1: Cognitive changes associated with Parkinson's disease dementia
It is important to note that cognitive changes in PD-D may have a distinct profile compared to other forms of dementia, such as Alzheimer's disease. Executive dysfunction, characterized by difficulties with planning, organizing, and decision-making, may be more prominent in PD-D [5]. Understanding these cognitive changes can help caregivers provide appropriate support and adapt their caregiving strategies to meet the needs of individuals with PD-D.
Behavioral and Emotional Symptoms
In addition to cognitive changes, individuals with PD-D may experience behavioral and emotional symptoms. Hallucinations, with visual hallucinations being more common than auditory ones, are prevalent in PD-D, affecting approximately 45% to 65% of individuals [5]. These hallucinations often involve complex, formed visions of people, animals, or objects. Delusions, particularly paranoid delusions, may also occur alongside hallucinations.
Mood changes and emotional fluctuations are common in PD-D. Individuals may experience depression, anxiety, irritability, and apathy. These emotional symptoms can have a significant impact on the well-being of both the individual with PD-D and their caregivers.
Behavioral and Emotional Symptoms
- Hallucinations (visual and auditory)
- Delusions, often paranoid
- Depression
- Anxiety
- Irritability
- Apathy
Table 2: Behavioral and emotional symptoms associated with Parkinson's disease dementia
Managing these behavioral and emotional symptoms requires a comprehensive approach that may involve medications, therapy, and support from healthcare professionals, caregivers, and support groups. It is essential for caregivers to provide a supportive and understanding environment for individuals with PD-D, addressing their emotional needs alongside their cognitive challenges.
By recognizing and understanding the symptoms and challenges associated with PD-D, caregivers and patients can navigate this complex condition with greater knowledge and empathy. Collaborating with healthcare professionals and implementing appropriate strategies and interventions can help enhance the quality of life for individuals living with PD-D.
Management and Treatment
When it comes to managing Parkinson's disease dementia, a combination of medications and lifestyle modifications can help improve symptoms and enhance the overall quality of life for individuals affected by the condition.
Medications and Therapies
Medications play a crucial role in managing the symptoms of Parkinson's disease dementia. Several medications commonly used for Parkinson's disease can also be beneficial in addressing the cognitive symptoms associated with Parkinson's disease dementia. Prescription medications developed for Alzheimer's disease, such as rivastigmine, donepezil, and galantamine, have demonstrated benefits in managing Parkinson's disease dementia. These medications aim to improve cognitive function and may be prescribed by healthcare professionals specialized in Parkinson's disease and dementia [4].
In addition to medications, other therapies may also be recommended. Physical therapy focusing on balance and stretching exercises can help individuals with Parkinson's disease dementia maintain their mobility and reduce the risk of falls. Working with a speech-language pathologist can assist in improving speech problems that may arise due to the condition. Moreover, regular aerobic exercise is strongly encouraged as it has been shown to have positive effects on Parkinson's disease symptoms. Additionally, some individuals with advanced Parkinson's disease may benefit from deep brain stimulation (DBS), a surgical procedure that involves implanting electrodes into specific areas of the brain to help manage symptoms such as tremors, rigidity, and involuntary movements.
Lifestyle Modifications
In addition to medication and therapy, lifestyle modifications can significantly contribute to the management of Parkinson's disease dementia. Healthy eating, regular exercise, and falls prevention strategies are emphasized. Incorporating aerobic exercise into a daily routine can have a positive impact on Parkinson's disease symptoms, including balance, flexibility, and muscle strength. Tai chi, a form of exercise originating from China, has been shown to improve flexibility, balance, and muscle strength, making it a beneficial option for individuals with Parkinson's disease.
To enhance the overall well-being of individuals with Parkinson's disease dementia, it is essential to focus on maintaining a healthy lifestyle. This includes a well-balanced diet, regular exercise, and adopting strategies to prevent falls. Caregivers and healthcare professionals can provide guidance and support in implementing these lifestyle modifications to optimize the management of Parkinson's disease dementia.
By combining medication and therapy with lifestyle modifications, individuals with Parkinson's disease dementia can better manage their symptoms and enjoy an improved quality of life. It is important to consult with healthcare professionals specializing in Parkinson's disease and dementia to develop an individualized treatment plan that addresses specific needs and challenges.
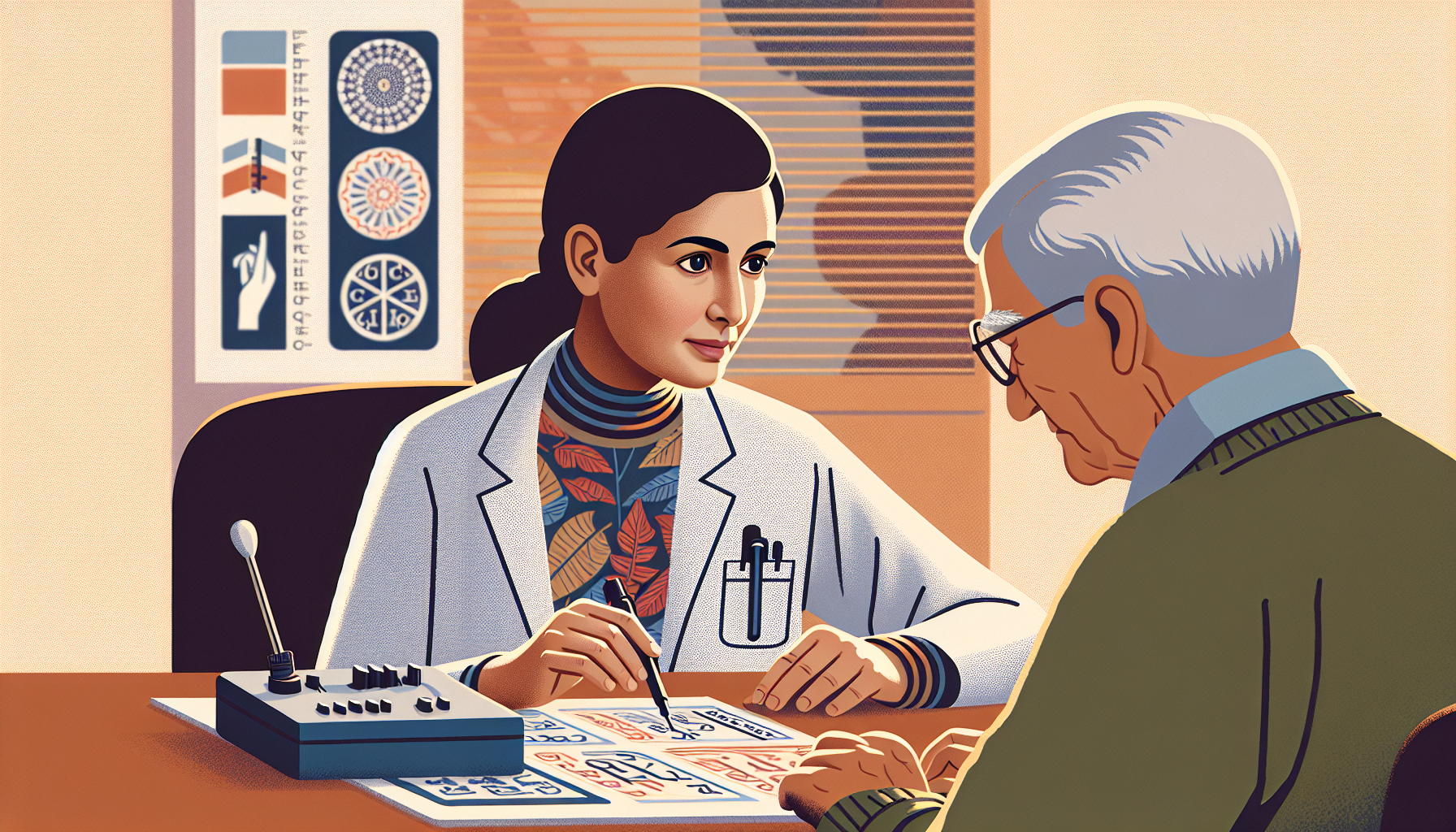
Diagnosis and Research
To accurately diagnose Parkinson's disease dementia (PD-D) and further research the condition, specific diagnostic criteria are utilized. These criteria help healthcare professionals assess the presence and frequency of dementia in late-stage Parkinson's disease patients. Let's explore the diagnostic criteria and advancements in diagnosis.
Diagnostic Criteria
The diagnostic criteria for Parkinson's disease dementia (PD-D) involve evaluating cognitive changes and determining their impact on daily functioning. Cognitive features associated with PD-D include impaired attention, executive functions, visuo-spatial functions, memory, and language. It is important to note that cognitive changes and the onset of dementia can vary from person to person.
Advancements in diagnostic criteria have shed light on the impact of clinical diagnostic criteria on the frequency of dementia in late-stage Parkinson's disease patients. A cross-sectional study conducted with 93 late-stage Parkinson's disease patients explored the frequency of dementia using various diagnostic criteria, including the MDS (Level I and II), DSM-IV, and DSM-5 criteria. The study found that the frequency of dementia in late-stage Parkinson's disease patients was partly dependent on the diagnostic criteria used, with significant discrepancies observed between different criteria. These findings emphasize the importance of considering different diagnostic criteria for accurate assessments and understanding the prevalence of dementia in patients with Parkinson's disease.
Advancements in Diagnosis
Research has shown that the average time from the onset of Parkinson's disease to the development of dementia is about 10 years. Furthermore, about three-quarters of people who live with Parkinson's for more than 10 years will develop dementia. Prior to the development of dementia, individuals may experience milder cognitive changes called mild cognitive impairment (MCI). Among those with normal cognition at Parkinson's diagnosis, about 30% will develop MCI after five years. However, the cognitive changes and their timing can vary from person to person.
Advancements in diagnostic techniques, such as neuroimaging, have contributed to a better understanding of Parkinson's disease dementia. Neuroimaging techniques, including structural imaging, have revealed structural changes in the brains of individuals with PD-D. These changes may include regional atrophy patterns, providing insights into the underlying neurodegenerative processes associated with the development of dementia.
By utilizing specific diagnostic criteria and advancements in diagnosis, healthcare professionals can better identify Parkinson's disease dementia and understand its impact on patients' lives. Continued research in this field aims to enhance diagnostic accuracy and develop targeted interventions to improve the quality of life for individuals living with PD-D.
Distinguishing Parkinson's Stages
As Parkinson's disease progresses, it can be helpful to distinguish between different stages to better understand the symptoms and provide appropriate care. There are two commonly recognized staging systems for Parkinson's disease: the Hoehn & Yahr stages and the Movement Disorder Task Force stages.
Hoehn & Yahr Stages
The Hoehn & Yahr staging system, established in 1967, defines five stages of Parkinson's disease based on the level of clinical disability. These stages help to assess the progression of the disease and guide treatment decisions.
These stages are a general guideline and may vary for each individual. It's important to note that the progression of Parkinson's disease can be different for everyone, and not all individuals will experience all stages.
Movement Disorder Task Force Stages
The Movement Disorder Task Force staging system recognizes three stages in early Parkinson's disease. This system takes into account the different phases of the disease, including the preclinical, prodromal, and clinical phases.
The Movement Disorder Task Force stages help to identify the early signs and symptoms of Parkinson's disease, allowing for early intervention and treatment.
These staging systems provide healthcare professionals and caregivers with a framework to understand the progression and severity of Parkinson's disease. However, it's important to remember that each individual's experience with the disease is unique, and the stages may not always align perfectly with an individual's symptoms or progression. Consulting with a healthcare provider specializing in Parkinson's disease can help in accurately assessing the stage and providing appropriate care and support.
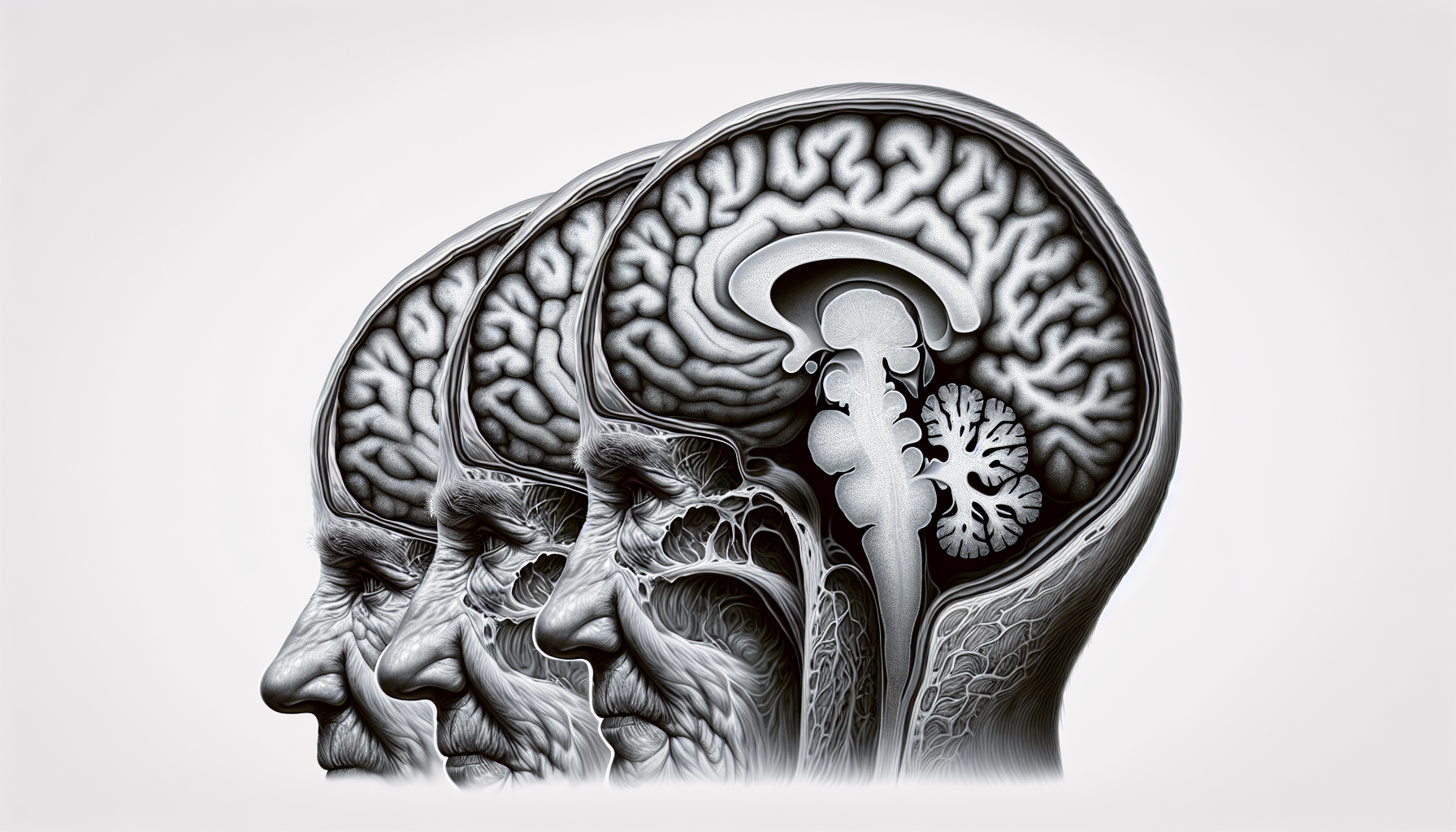
Insights from Neuroimaging
Neuroimaging techniques have provided valuable insights into Parkinson's Disease Dementia (PD-D), shedding light on the structural changes that occur in the brain. These imaging studies have helped in understanding the progression and distinguishing features of PD-D.
Structural Changes
Studies using neuroimaging have revealed that individuals with PD-D exhibit whole brain and regional structural changes. These changes include greater rates of whole brain atrophy and regional atrophy in specific areas of the brain, such as the temporal lobe. Atrophy refers to the shrinkage or loss of brain tissue.
Regional Atrophy Patterns
It is important to note that there is an overlap in the pattern of regional atrophy between PD-D, Parkinson's Disease (PD), and Dementia with Lewy Bodies (DLB). This overlap poses a challenge in differentiating PD-D from other conditions solely based on structural changes observed through neuroimaging.
By studying the structural changes and regional atrophy patterns in the brains of individuals with PD-D, researchers aim to better understand the underlying mechanisms of the disease and develop more accurate diagnostic tools.
While neuroimaging provides valuable insights, it is important to note that these findings are just one piece of the puzzle. Diagnosis and management of PD-D require a comprehensive evaluation by healthcare professionals, considering both clinical symptoms and neuroimaging findings. Neuroimaging is a powerful tool that continues to contribute to our understanding of PD-D and may aid in future advancements in diagnosis and treatment.
References
[1]: https://www.healthline.com/health/parkinsons/parkinsons-dementia
[2]: https://www.alz.org/alzheimers-dementia/what-is-dementia/types-of-dementia/parkinson-s-disease-dementia
[3]: https://www.parkinson.org/understanding-parkinsons/non-movement-symptoms/dementia
[4]: https://www.hopkinsmedicine.org/health/conditions-and-diseases/parkinsons-disease/parkinsons-disease-and-dementia
[5]: https://movementdisorders.onlinelibrary.wiley.com/doi/10.1002/mds.21507
[6]: https://www.mayoclinic.org/diseases-conditions/parkinsons-disease/diagnosis-treatment/drc-20376062
[7]: https://www.frontiersin.org/articles/10.3389/fneur.2021.652424/full