Home Health Care Services Covered By Medicare
Get the comprehensive guide to Medicare-covered home health care services for seniors. Learn about the services and how to qualify today!
.jpg)
Home Health Care Services Covered By Medicare
When it comes to home health care services, understanding what is covered by Medicare is essential. Medicare is a federal health insurance program in the United States that primarily serves individuals aged 65 and older, as well as certain younger individuals with disabilities. It is divided into different parts, with Part A and Part B being the primary components relevant to home health care coverage.

What is Medicare?
Medicare is a government-funded program that provides health insurance to eligible individuals. It is designed to help cover the costs of various medical services, including hospital stays, doctor visits, prescription drugs, and home health care. Medicare is divided into different parts:
- Medicare Part A: Also known as hospital insurance, Part A covers inpatient hospital care, skilled nursing facility care, hospice care, and limited home health care services.
- Medicare Part B: Also known as medical insurance, Part B covers outpatient care, doctor visits, preventive services, and medically necessary home health care services.
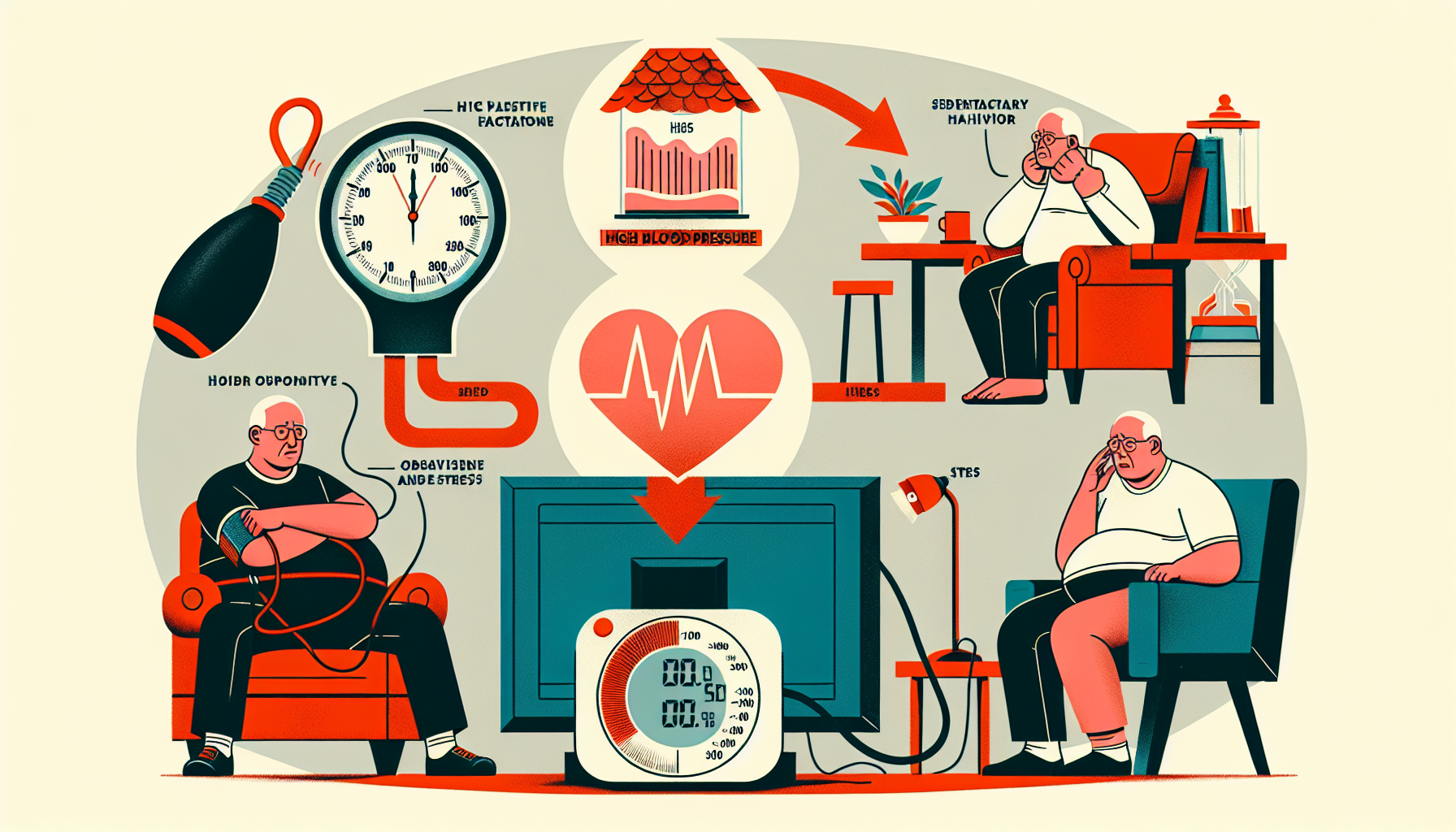
Coverage for Home Health Care Services
Medicare provides coverage for certain home health care services, allowing eligible individuals to receive necessary care in the comfort of their own homes. To qualify for coverage, the following conditions must be met:
- The individual must be under the care of a doctor who has established a plan of care.
- The individual must require skilled nursing care or therapy services on an intermittent basis.
- The home health agency providing the services must be Medicare-certified.
Home health care services covered by Medicare include:
Medicare has specific guidelines and requirements for coverage of home health care services. These guidelines include limitations on the frequency and duration of services, as well as the need for a qualifying condition and physician certification.
Understanding the coverage provided by Medicare for home health care services is crucial for individuals seeking care in their own homes. By knowing what is included and the requirements for coverage, individuals can make informed decisions about their health care options.
Skilled Nursing Care
Skilled nursing care is an essential component of Medicare-approved home health care services. Skilled nurses provide specialized care and support to individuals who require medical assistance in the comfort of their own homes.
Services Provided
Skilled nursing care encompasses a wide range of services delivered by licensed and trained nurses. These services may include:
- Wound care and dressing changes
- Administering medication
- Intravenous (IV) therapy
- Monitoring vital signs
- Catheter care
- Rehabilitation support
- Disease management and education
- Managing chronic conditions
- Post-surgical care
- Pain management
The specific services provided will depend on the individual's needs and the care plan developed by the healthcare team.
Eligibility and Coverage
To be eligible for skilled nursing care covered by Medicare, certain criteria must be met. The individual must be:
- Enrolled in Medicare Part A and/or Part B
- Under the care of a physician who has certified the need for skilled nursing care
- Homebound, meaning leaving home requires a considerable and taxing effort
Medicare Part A covers skilled nursing care for individuals who have a qualifying hospital stay of at least three consecutive days and are admitted to a Medicare-certified skilled nursing facility. On the other hand, Medicare Part B covers skilled nursing care provided at home.
Medicare covers skilled nursing care on an intermittent basis, meaning it is provided for a short and specific period of time. The need for skilled nursing care should be temporary, and the care should be aimed at improving or maintaining the individual's health condition.
Understanding the services and eligibility criteria for skilled nursing care can help individuals make informed decisions about their home health care needs. By partnering with Medicare-certified home health care providers, individuals can access the skilled nursing care they require in the familiar and comfortable environment of their own homes.
Physical Therapy
Physical therapy is an essential component of home health care services covered by Medicare. It focuses on improving and restoring physical function, mobility, and overall quality of life. Whether you're recovering from surgery, managing a chronic condition, or rehabilitating after an injury, physical therapy can play a crucial role in your recovery process.
Services Provided
Under Medicare-approved home health care services, physical therapy can include a range of treatments and interventions tailored to your specific needs. Some of the services provided by physical therapists may include:
- Evaluation and assessment of your physical condition and functional abilities.
- Development of a personalized treatment plan to address your specific goals and needs.
- Therapeutic exercises targeting strength, flexibility, and balance.
- Manual therapy techniques to improve joint mobility and reduce pain.
- Gait training and assistance with walking aids, if necessary.
- Education on proper body mechanics and injury prevention.
- Assistance with adaptive equipment and assistive devices.
- Monitoring and tracking your progress throughout the course of treatment.
The specific services provided may vary based on your individual condition and the recommendations of your healthcare team.
Eligibility and Coverage
To be eligible for Medicare coverage of physical therapy as part of home health care services, certain criteria must be met. These criteria include:
- Being enrolled in Medicare Part A and/or Part B.
- Having a medical need for skilled care, meaning that the services must be provided by a qualified healthcare professional under a plan of care established by your doctor.
- Meeting the homebound requirement, which means that your condition must be such that it is difficult for you to leave your home without assistance.
Under Medicare, physical therapy services are typically covered up to a certain limit. This limit may change from year to year, so it's important to stay updated on the latest guidelines. Medicare also has specific guidelines regarding the frequency and duration of physical therapy services. It's crucial to work closely with your healthcare team to ensure that the services provided align with Medicare's coverage criteria.
Physical therapy, as part of Medicare-approved home health care services, can be instrumental in helping you regain and maintain your physical well-being. By working closely with your healthcare team and adhering to Medicare guidelines, you can receive the necessary physical therapy services to support your recovery and enhance your overall quality of life.
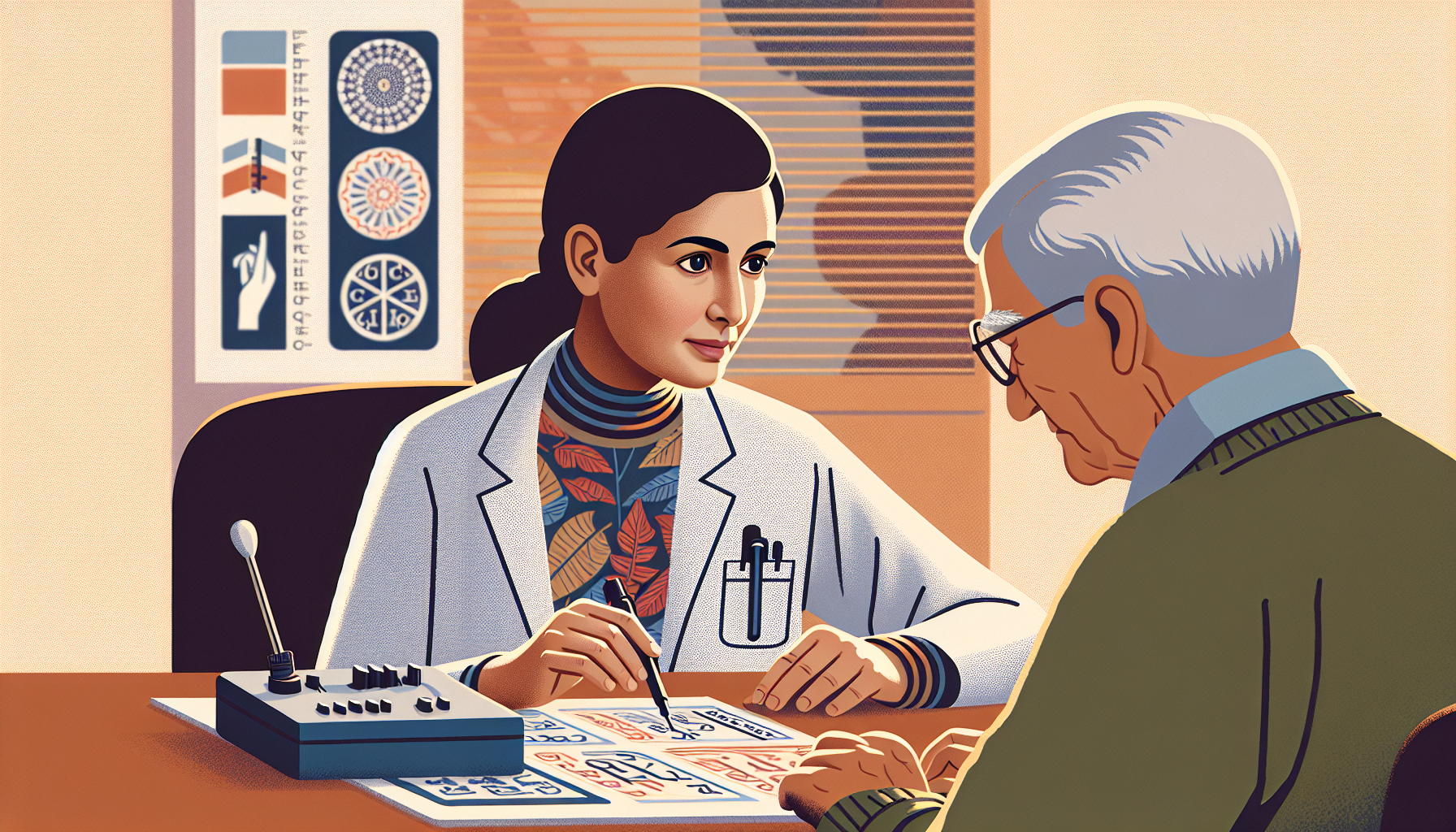
Occupational Therapy
Occupational therapy is an essential component of Medicare-approved home health care services. It focuses on helping individuals regain or develop the necessary skills to perform activities of daily living independently. Whether it's improving mobility, enhancing coordination, or adapting to physical limitations, occupational therapy plays a vital role in promoting overall well-being and independence.
Services Provided
Occupational therapy services encompass a wide range of interventions tailored to meet the unique needs of each individual. Some of the key services provided by occupational therapists include:
- Assessment and Evaluation: Occupational therapists assess the individual's functional abilities, home environment, and specific challenges to develop a personalized treatment plan.
- Adaptive Equipment and Assistive Devices: Occupational therapists may recommend and train individuals on the use of adaptive equipment or assistive devices to enhance independence in daily activities.
- Therapeutic Exercises: Occupational therapists guide individuals through therapeutic exercises to improve strength, flexibility, coordination, and endurance.
- Activities of Daily Living (ADL) Training: Occupational therapists focus on specific ADLs such as dressing, bathing, grooming, and feeding, helping individuals regain or enhance their ability to perform these tasks independently.
- Cognitive Rehabilitation: Occupational therapists work with individuals to improve cognitive skills such as memory, attention, problem-solving, and decision-making.
- Environmental Modifications: Occupational therapists may recommend modifications to the home environment to ensure it is safe and accessible, reducing the risk of falls or other accidents.
Eligibility and Coverage
To be eligible for occupational therapy services under Medicare, certain criteria must be met. Individuals must have a referral from a healthcare provider, and the services must be deemed medically necessary. Additionally, the individual must be under the care of a doctor who establishes and periodically reviews the plan of care.
Medicare Part B typically covers occupational therapy services when provided by a Medicare-approved home health agency. Coverage includes evaluation, treatment, and follow-up services. However, Medicare may have certain limitations and requirements regarding the frequency and duration of services.
Understanding the services provided and the eligibility criteria for occupational therapy is crucial for individuals seeking Medicare-approved home health care services. By working with a Medicare-approved home health agency, individuals can access the necessary support and expertise to enhance their functional abilities and improve their overall quality of life.
Speech-Language Pathology Services
Speech-Language Pathology (SLP) services play a vital role in home health care, helping individuals with speech, language, and swallowing disorders regain their communication skills and improve their quality of life. Medicare provides coverage for these essential services, ensuring that eligible individuals have access to the necessary care they need.
Services Provided
Speech-Language Pathology services encompass a range of evaluations, treatments, and interventions tailored to address specific communication and swallowing needs. Some of the services provided by SLPs include:
- Speech Evaluation and Therapy: SLPs assess and treat speech disorders, such as articulation difficulties, fluency disorders, and voice disorders. Therapy techniques may include exercises to improve speech clarity, breathing exercises, and vocal hygiene education.
- Language Evaluation and Therapy: SLPs evaluate and treat language disorders, including difficulties with comprehension, expression, and social communication. Therapy may involve exercises to improve vocabulary, grammar, and conversational skills.
- Swallowing Evaluation and Therapy: SLPs specialize in assessing and treating swallowing disorders (dysphagia). They evaluate the individual's ability to safely swallow food and liquids and develop personalized treatment plans to improve swallowing function.
Eligibility and Coverage
To be eligible for Medicare coverage of Speech-Language Pathology services, the following criteria must be met:
- Homebound Status: The individual must have a condition that makes it difficult to leave their home without assistance.
- Physician's Order: A physician must prescribe Speech-Language Pathology services as part of the patient's plan of care.
- Medical Necessity: The services provided by an SLP must be deemed medically necessary to treat a speech, language, or swallowing disorder.
Medicare typically covers 80% of the approved amount for Speech-Language Pathology services. The remaining 20% is the responsibility of the individual or their secondary insurance. Deductibles and co-pays may apply.
By providing coverage for Speech-Language Pathology services, Medicare ensures that individuals with communication and swallowing difficulties can access the necessary care in the comfort of their own homes. If you or a loved one requires these services, consult with a qualified healthcare provider to determine eligibility and develop a personalized plan of care.
Medical Social Services
Medical social services play a vital role in Medicare-approved home health care services by providing support and assistance to patients and their families. These services focus on addressing social and emotional factors that can impact an individual's well-being and overall health. Let's explore the services provided and the eligibility and coverage for medical social services.
Services Provided
Medical social services encompass a wide range of support and assistance to meet the unique needs of each patient. Some of the services provided include:
- Assessing the patient's social and emotional needs: A medical social worker evaluates the patient's social and emotional well-being to identify any areas that may require attention or support.
- Counseling and emotional support: Medical social workers offer counseling services to patients and their families, helping them navigate the emotional challenges that may arise during their healthcare journey.
- Assistance with community resources: Medical social workers connect patients and their families with community resources and support services, such as support groups, transportation assistance, and financial aid programs.
- Advance care planning: Medical social workers facilitate discussions on advance care planning, helping patients and their families make informed decisions about their healthcare preferences and end-of-life care.
- Support for caregiver stress: Medical social workers provide guidance and support to caregivers, helping them cope with the stress and challenges of caring for a loved one.
Eligibility and Coverage
To be eligible for medical social services under Medicare-approved home health care, certain criteria must be met. The patient must require skilled care, and a physician must certify the need for home health services. Additionally, the patient's condition should be such that the services provided by a medical social worker are necessary for the treatment and management of the patient's illness or injury.
Medicare covers medical social services as part of its home health care benefits. The coverage typically includes the services provided by a medical social worker as well as any related supplies and equipment needed to carry out these services. Medicare coverage may have limitations and specific requirements, such as the need for intermittent skilled nursing care or therapy services.
Understanding the benefits, guidelines, and requirements of Medicare home health care will help you make informed decisions regarding the services you or your loved one may need.
By including medical social services in Medicare-approved home health care, patients can receive the necessary support and assistance to address their social and emotional needs, enhancing their overall well-being and quality of life. The expertise of medical social workers can make a significant difference in the holistic care provided to individuals receiving home health care services.
Home Health Aide Services
When it comes to home health care services covered by Medicare, one important component is the provision of Home Health Aide (HHA) services. These services aim to assist individuals with their daily activities and personal care needs in the comfort of their own homes. Let's explore the services provided by Home Health Aides and the eligibility and coverage criteria.
Services Provided
Home Health Aides are trained professionals who provide essential personal care services to individuals in need. Some of the services they offer include:
- Assistance with bathing, grooming, and dressing
- Help with mobility and transferring
- Support with toileting and incontinence care
- Meal preparation and assistance with feeding
- Light housekeeping and laundry
- Medication reminders
- Companionship and emotional support
Home Health Aides play a crucial role in ensuring the well-being and comfort of individuals who may have difficulty performing these tasks independently. Their compassionate care helps promote independence and enhances the overall quality of life for those receiving their services.
Eligibility and Coverage
To be eligible for Home Health Aide services covered by Medicare, certain criteria must be met. The individual must:
- Be under the care of a doctor who has established and regularly reviews a plan of care.
- Require skilled nursing care, physical therapy, or speech-language pathology services on an intermittent basis.
- Be homebound, which means leaving home requires a considerable effort and is infrequent.
Under Medicare, coverage for Home Health Aide services is typically provided as part of the broader home health care benefit. It's important to note that coverage for Home Health Aide services is generally limited to individuals who also require skilled nursing care or therapy services. Medicare may cover up to 35 hours per week of Home Health Aide services, depending on the individual's needs and the doctor's plan of care.
It's essential to consult with your healthcare provider and review the specific guidelines and requirements outlined by Medicare to determine your eligibility and coverage for Home Health Aide services.
By understanding the services provided by Home Health Aides and the eligibility and coverage criteria, individuals can make informed decisions about their home health care needs. Remember to consult with your healthcare provider and explore the resources available to you to ensure you receive the appropriate care and support at home.
Coverage Limitations and Requirements
While Medicare provides coverage for a range of home health care services, it's important to understand the limitations and requirements associated with this coverage. This section will outline the frequency and duration of services, as well as the qualifying conditions and physician certification needed for Medicare-approved home health care services.
Frequency and Duration of Services
Medicare coverage for home health care services is based on the needs and condition of the individual. The frequency and duration of services are determined by a qualified healthcare professional and are subject to certain limitations. It's important to note that Medicare coverage for home health care services is intended for short-term, intermittent care rather than long-term or continuous care.
The frequency of home health care visits will depend on the individual's specific needs and the care plan developed by the healthcare professional. Medicare typically covers services provided a few times per week, but in certain cases, daily visits may be approved when medically necessary. The duration of services is also determined based on the individual's condition and progress. Medicare coverage for home health care services is typically provided for a limited period, and the need for ongoing services is reassessed periodically.
Qualifying Conditions and Physician Certification
To be eligible for Medicare coverage of home health care services, certain conditions must be met. Medicare requires the individual to be homebound, meaning that leaving the home requires a considerable and taxing effort. Additionally, the individual must require skilled nursing care, physical therapy, or speech-language pathology services on an intermittent basis.
Furthermore, Medicare requires a physician's certification to confirm the need for home health care services. The physician must establish and periodically review a plan of care, outlining the specific services required and the expected outcomes. This certification is crucial in determining the eligibility and coverage for home health care services under Medicare.
It's important to consult with healthcare professionals and Medicare resources to understand the specific coverage limitations and requirements for home health care services.
Navigating the world of Medicare-approved home health care services can be complex, but understanding the coverage limitations and requirements can help individuals make informed decisions about their healthcare options.
FAQs
How often can I receive home health care services?
The frequency of your home health care services will depend on your specific needs and the care plan developed by your doctor and home health care team. However, Medicare typically covers up to 28 hours of home health care per week.
Can I choose my own home health care provider?
Yes, you have the right to choose your own home health care provider as long as they are Medicare-certified.
Will I have to pay anything out-of-pocket for my home health care services?
If you meet the eligibility criteria for Medicare-covered home health care services, you generally won't have to pay anything out-of-pocket. However, if you require medical equipment or supplies that aren't covered by Medicare, you may be responsible for paying for those items.