How Long Will Medicaid Pay For Home Care?
In this article, we will delve into the intricacies of Medicaid's home care coverage, including eligibility, services, and the factors influencing how long Medicaid will pay for these services.
.jpg)
How Long Will Medicaid Pay For Home Care?
Medicaid home care is a program that provides financial assistance for eligible individuals who require care and support in their own homes. It is designed to help individuals who may have difficulty performing daily activities due to age, disability, or medical conditions. Medicaid home care allows individuals to receive the necessary care while remaining in the comfort and familiarity of their own homes.
The specific services covered by Medicaid home care vary by state and individual needs. However, common services may include assistance with personal hygiene, meal preparation, medication management, light housekeeping, and companionship. Medicaid home care is different from Medicare, which primarily covers medical services and is available to individuals aged 65 and older or those with certain disabilities.
Benefits of Medicaid Home Care
Medicaid home care offers several benefits for individuals and families. Some of the key advantages include:
- Cost-Effective: Medicaid home care can significantly reduce the financial burden associated with long-term care. By providing financial assistance for home-based services, it enables individuals to receive the care they need without incurring high costs.
- Personalized Care: Home care allows individuals to receive personalized care tailored to their specific needs. The services provided are based on an individual's assessment, ensuring that they receive the appropriate level of care and support.
- Independence and Comfort: Medicaid home care enables individuals to maintain their independence and stay in the comfort of their own homes. This can have a positive impact on their overall well-being and quality of life.
- Family Involvement: Medicaid home care recognizes the importance of family involvement in the care process. It allows family members to actively participate in the care of their loved ones, fostering a sense of connection and support.
- Continuity of Care: By receiving care at home, individuals can benefit from continuity of care. They can establish a long-term relationship with their care providers, ensuring consistency and familiarity in their care journey.
Understanding the basics of Medicaid home care is the first step in accessing the benefits it offers. It is important to consult with your state's Medicaid program or a professional healthcare provider to determine eligibility and specific coverage details. By exploring the resources available, you can make informed decisions and access the support you need.
Duration of Medicaid Home Care
When considering how long Medicaid will pay for home care, it's important to understand the factors that can affect the duration of coverage and the limits associated with Medicaid home care.
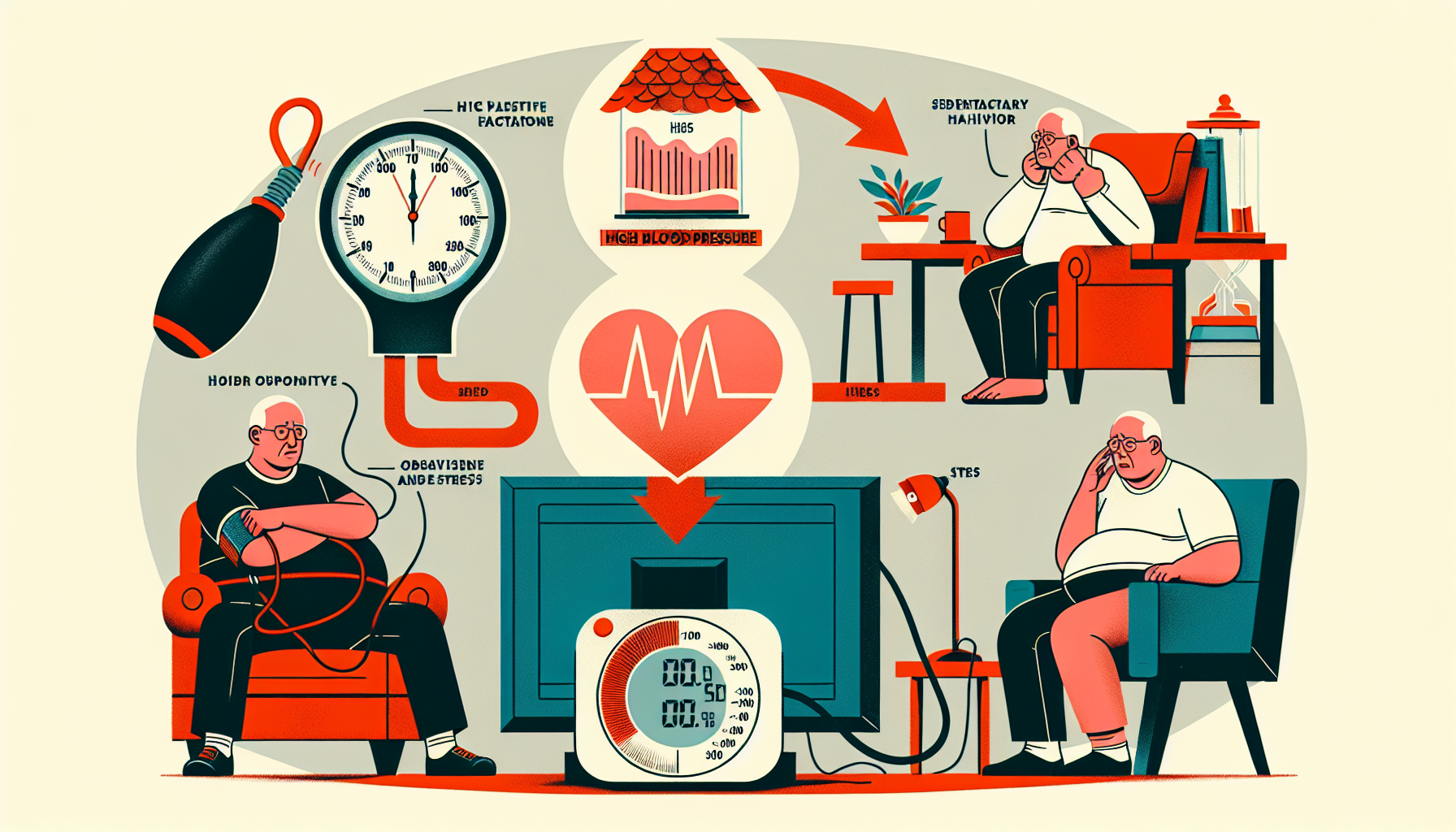
Factors Affecting Medicaid Home Care Duration
The duration of Medicaid home care can vary depending on several factors. These factors may include the individual's medical condition, level of care required, and the specific guidelines set by the state Medicaid program.
The primary factor that influences the duration of Medicaid home care is the individual's medical condition. Medicaid home care is typically provided to individuals who have a medical need for assistance with activities of daily living (ADLs) or skilled nursing care. The severity of the medical condition and the prognosis for improvement may play a role in determining the length of time that Medicaid will cover home care services.
Additionally, the level of care required can impact the duration of Medicaid home care. Medicaid may provide different levels of care, ranging from basic assistance with daily tasks to skilled nursing care. The level of care required will be assessed during the initial Medicaid home care assessment, which helps determine the appropriate services and duration of coverage.
Medicaid Home Care Coverage Limits
Medicaid home care coverage limits vary by state and may be subject to certain guidelines and regulations. Each state's Medicaid program sets specific limits on the duration of home care services that they will cover. These limits may be based on factors such as the individual's medical condition, level of need, and available funding.
Medicaid home care coverage may have time limits or specific requirements for recertification. Recertification is a process where the individual's eligibility for Medicaid home care is reassessed to ensure continued medical necessity. The frequency of recertification varies by state and may depend on the individual's specific circumstances.
To gain a better understanding of the Medicaid home care coverage duration and specific limitations in your state, it is recommended to consult your state's Medicaid program or eligibility office. They can provide detailed information on the coverage period and any time limits that may apply.
By understanding the factors that affect the duration of Medicaid home care and being aware of any coverage limits, individuals and their families can better plan and make informed decisions regarding their long-term care needs.
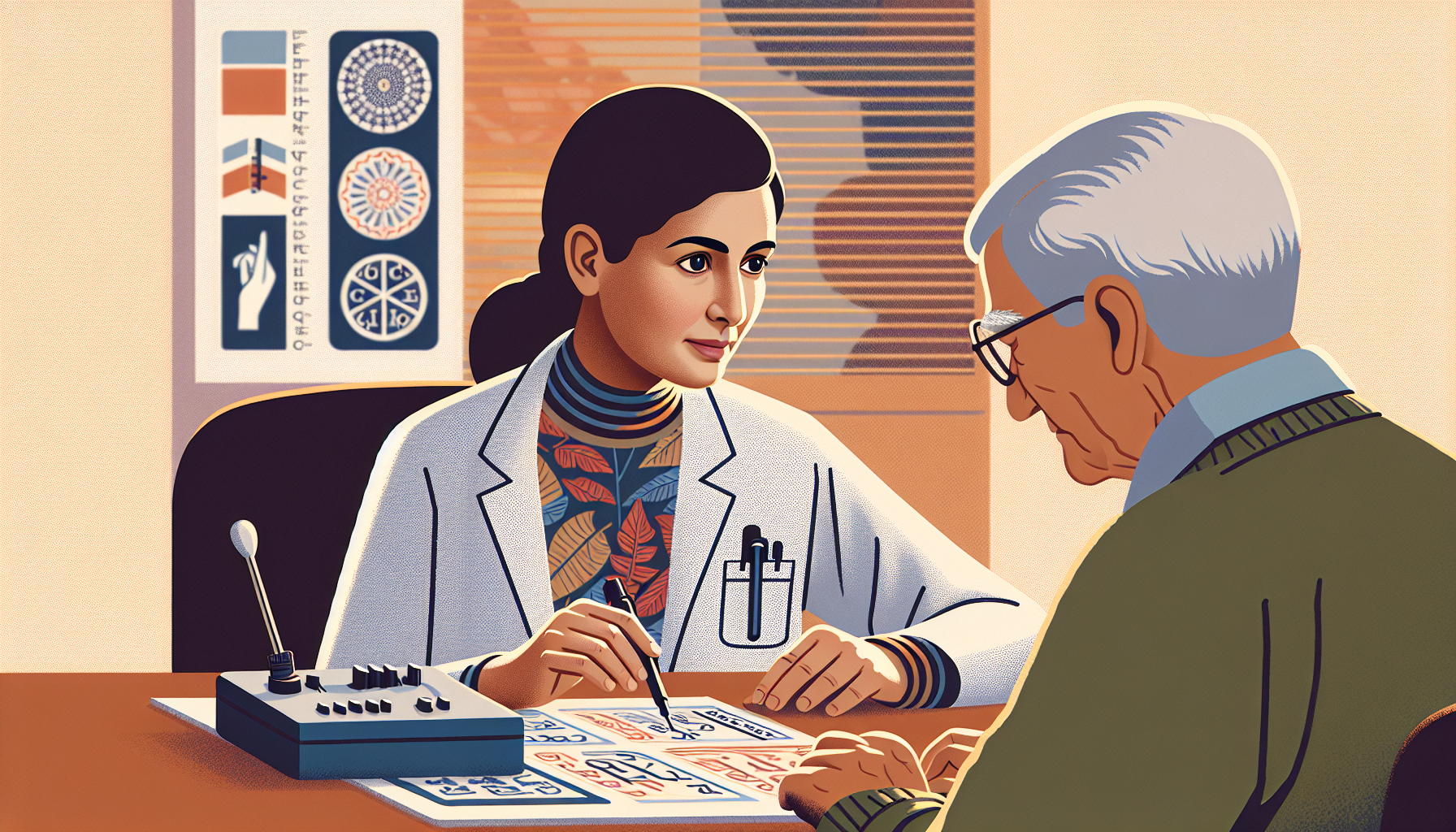
Initial Medicaid Home Care Assessment
Before receiving Medicaid home care, an initial assessment is conducted to determine the individual's eligibility and the level of care required. This assessment plays a crucial role in ensuring that the right services are provided to meet the patient's specific needs. Let's explore the two key aspects of this assessment: assessing the need for home care and determining the level of care required.
Assessing the Need for Home Care
During the initial assessment, a healthcare professional evaluates the individual's medical condition, functional abilities, and overall health to determine if home care is necessary. This assessment involves a comprehensive review of the individual's medical history, current health status, and any ongoing treatments or medications.
The healthcare professional will also assess the individual's ability to perform activities of daily living (ADLs), such as bathing, dressing, eating, and mobility. They will evaluate the individual's level of independence and identify any difficulties or limitations they may have. This assessment helps determine if the individual requires assistance and support to safely manage these activities at home.
In addition to ADLs, the assessment may also consider instrumental activities of daily living (IADLs) such as meal preparation, housekeeping, and managing finances. These activities are important for maintaining a safe and comfortable living environment.
Determining the Level of Care Required
Once the need for home care has been established, the next step is to determine the appropriate level of care required. This determination is based on the individual's assessed needs and the specific services and support they require.
The level of care can range from minimal assistance with activities of daily living to more extensive support, such as skilled nursing care or therapy services. The assessment takes into account the individual's medical condition, the complexity of their care needs, and any specialized services that may be required.
The level of care is typically defined by Medicaid guidelines and criteria. These guidelines ensure that the level of care provided is appropriate and necessary for the individual's health and well-being. The level of care may be subject to periodic reassessment to ensure that it aligns with the individual's changing needs over time.
By conducting a thorough initial assessment, Medicaid aims to ensure that the home care services provided are tailored to the individual's specific needs. This assessment process helps determine the eligibility for Medicaid home care and ensures that the level of care is appropriate and beneficial.
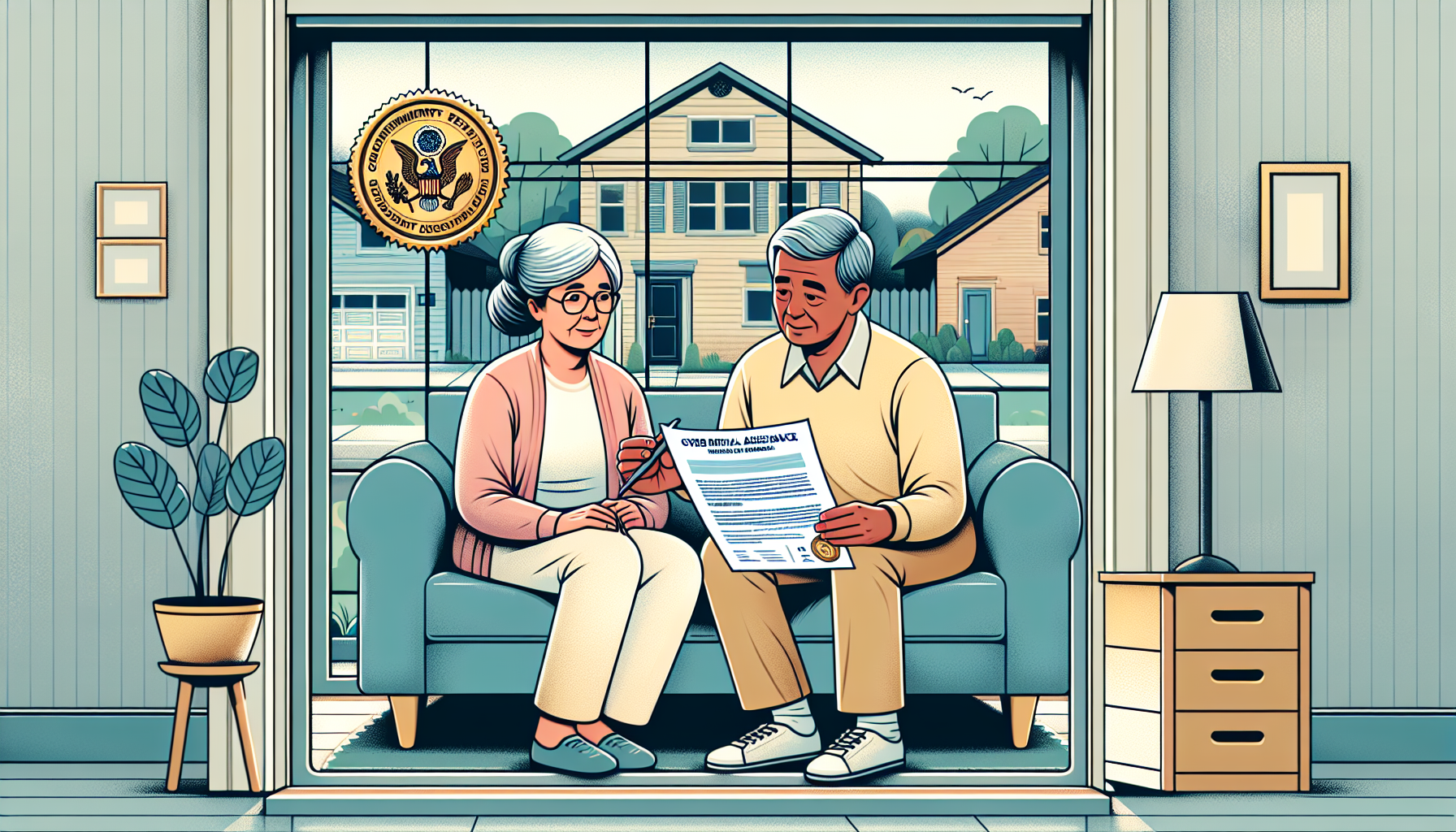
Medicaid Home Care Recertification
Once approved for Medicaid home care, recipients will need to go through a recertification process to determine their ongoing eligibility for continued coverage. This ensures that individuals receive the necessary care and support for their specific needs. Let's explore the recertification process and the frequency at which it occurs.
Recertification Process
During the recertification process, a comprehensive evaluation is conducted to assess the individual's current condition and determine if they still meet the criteria for Medicaid home care. This assessment typically involves a review of the recipient's medical records, a physical examination, and a discussion of their care needs.
The specific steps and requirements for recertification may vary depending on the state and the Medicaid program. It's essential to consult the local Medicaid office or a healthcare professional to understand the recertification process in your area.
Frequency of Recertification
The frequency of Medicaid home care recertification also varies by state and individual circumstances. In general, recertification is required at regular intervals to ensure that the recipient's needs are still being met and that they continue to meet the eligibility criteria for Medicaid home care.
Recertification periods can range from every six months to annually. Some states may require more frequent recertification for individuals with more complex care needs, while others may have longer intervals for those with stable conditions.
To find out the specific recertification period for Medicaid home care in your state, it is essential to reach out to the local Medicaid office or refer to the official Medicaid guidelines.
Understanding the recertification process and the frequency of recertification is crucial for individuals receiving Medicaid home care. By staying informed and prepared for the recertification process, recipients and their families can ensure continued coverage and access to the necessary care and services.
Medicaid Home Care Exceptions and Extensions
While Medicaid home care has coverage limits, there are exceptions and extensions available for certain circumstances. These exceptions and extensions provide additional support and flexibility beyond the standard duration of Medicaid home care.
Exceptions to Medicaid Home Care Limits
In some cases, exceptions may be made to the usual limits of Medicaid home care coverage. These exceptions are typically granted when there are specific medical or functional needs that require extended care. Common exceptions include:
- Medical Necessity: Medicaid may extend the duration of home care if the individual's medical condition necessitates ongoing care at home. This could apply to individuals with chronic illnesses, severe disabilities, or complex medical needs.
- Disability: Individuals with disabilities may be eligible for an exception to the standard coverage limits. This recognizes that their care needs may be ongoing and require long-term support.
- Special Circumstances: Medicaid may consider exceptions for individuals facing unique circumstances that require extended home care. This could include situations such as end-of-life care, palliative care, or individuals in need of specialized care due to a catastrophic event.
Exceptions to Medicaid home care limits are evaluated on a case-by-case basis. The specific criteria for exceptions may vary by state. To understand the exceptions available in your state, it is advisable to check with your local Medicaid office or consult with a Medicaid specialist.
Extensions for Special Circumstances
In addition to exceptions, Medicaid also provides extensions for special circumstances that may require additional home care beyond the standard coverage period. These extensions are typically granted when there is a temporary change in the individual's care needs. Common situations that may warrant an extension include:
- Post-Hospitalization: Individuals who require additional home care support following a hospital stay may be eligible for an extension. This allows for continued care during the recovery and rehabilitation period.
- Transitional Care: Medicaid may provide extensions for individuals transitioning from a higher level of care, such as a nursing facility, to home care. This ensures a smooth and gradual transition while maintaining necessary support.
- Change in Condition: If there is a significant change in the individual's condition that requires increased care temporarily, an extension may be granted to ensure adequate support during this period.
Extensions for special circumstances are typically time-limited and may require periodic reassessments to determine the continued need for home care.
Navigating the duration of Medicaid home care can be complex, but understanding the exceptions and extensions available can help ensure that individuals receive the necessary support for their specific care needs. By planning ahead and exploring alternative care options, individuals and their families can make informed decisions about their long-term care.
Planning Ahead for Medicaid Home Care
When it comes to Medicaid home care, it's essential to plan ahead to ensure that you or your loved one receives the necessary care for the duration needed. This includes considering long-term care planning and exploring alternative care options. By understanding these aspects, you can make informed decisions and ensure the best possible care.
Long-Term Care Planning
Long-term care planning involves assessing your current and future needs and considering the available options for care. It's important to start planning early, even before the need for Medicaid home care arises. This allows you to explore different care settings, such as home care, assisted living, or nursing homes, and determine which option aligns best with your goals and preferences.
During the planning process, it's crucial to consult with professionals who specialize in long-term care, such as social workers or elder law attorneys. They can provide guidance on understanding Medicaid eligibility criteria, financial planning, and available resources. Long-term care planning helps you navigate the complexities of the Medicaid system and ensures that you can access the care you need when the time comes.
Exploring Alternative Care Options
While Medicaid home care provides valuable assistance, it's beneficial to explore alternative care options as well. Depending on your circumstances and needs, there may be other services and programs available that complement or supplement Medicaid home care.
Some alternative care options to consider include:
- Adult Day Care: Adult day care centers provide a supportive and engaging environment for individuals who require care during the day. They offer social activities, meals, and personal care assistance, allowing caregivers to have respite while ensuring their loved ones receive proper care.
- Respite Care: Respite care provides temporary relief to primary caregivers. It can range from a few hours to several days and is designed to give caregivers a break from their caregiving responsibilities. Respite care can be provided in a variety of settings, including the home or a residential facility.
- Assisted Living: Assisted living facilities offer a combination of housing, personal care services, and support. They are ideal for individuals who require assistance with activities of daily living but do not need the level of care provided in a nursing home. Assisted living facilities provide a community-like environment with social activities and 24-hour support.
- Nursing Homes: Nursing homes are suitable for individuals with complex medical needs who require round-the-clock care. These facilities provide skilled nursing care, rehabilitation services, and assistance with daily activities. Medicaid may also cover nursing home care if it is deemed medically necessary.
By exploring these alternative care options, you can find the right combination of services that meet your specific needs. It's important to discuss these options with your healthcare provider and Medicaid case manager to ensure that you have a comprehensive care plan in place.
Planning ahead for Medicaid home care involves considering your long-term care needs and exploring different care options. By doing so, you can make informed decisions, optimize the benefits of Medicaid home care, and ensure that you or your loved one receives the necessary care for the required duration.